The article explains the risk of occurrence of Rhesus-conflict during pregnancy. Recommendations are given to prospective parents on the prevention of possible complications.
Contents of
- How is Rh factor determined?
- Blood group compatibility chart
- Symptoms of rhesus conflict
- Cause of rhesus conflict:
- Blood test for Rh factor
- What do antibodies mean?
- Rhesus conflict in second and subsequent pregnancies
- Maximum risk for women
- Consequences of rhesus conflict for fetus
- Treatment of rhesus conflict
- Video: about Rhesus factor and threat to child
Pregnant women become registered in a female consultation. She has to undergo a lot of examinations, take tests. Obligatory will be an analysis that will help determine the blood groups of future parents and their Rh factors.
Rh factor is a specific property of human erythrocytes, which is due to the presence of an antigen protein. Other group systems do not affect the presence of Rh factor in the blood. Every person is born with a certain Rh factor. He remains unchanged until his death and is inherited by children.

How is the Rh factor determined?
The Rh factor in medicine is indicated by the combination of two Latin letters Rh. If Rhesus antigen is detected in red blood cells, then the blood of such a person is considered Rh-positive( Rh +).There are about 85% of such people in the world. The remaining 15% are carriers of Rh-negative blood
. The owners of negative rhesus do not experience any particular inconveniences and are not considered sick. But if a woman is going to become a mother, then she needs special attention.
If the antigen and antibody of the same name are present in the blood, then their combination leads to the adhesion of the red blood cells
. The glued red blood cells are unable to perform the function of oxygen delivery. In the bloodstream of healthy people, antigen and antibody of the same name are not found.
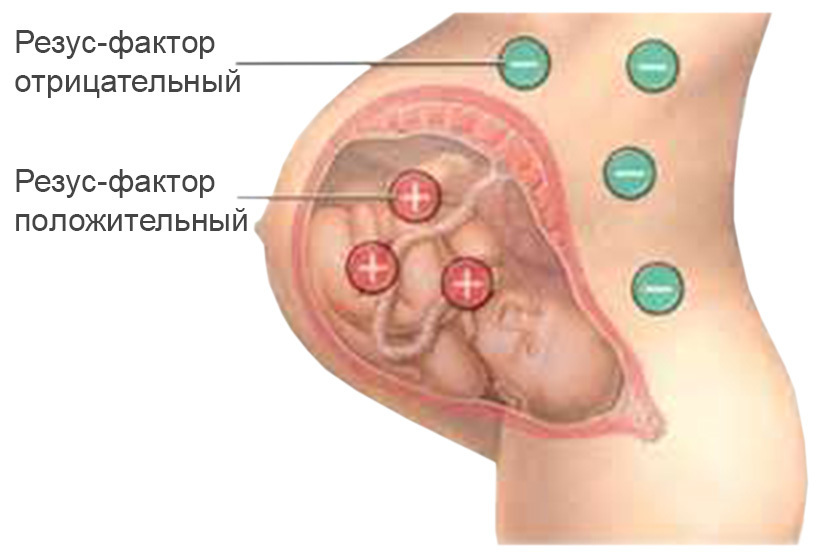
Rh-conflict is observed when Rh-positive blood is mixed with Rh-negative. Fetal blood becomes incompatible with the blood of the mother. All systems of the mother's organism will fight against the foreign protein
appearing in it. This happens when the father's Rh ressus is inherited, with the immunological incompatibility of blood groups: maternal and child. With incompatibility of blood groups, there is less danger than with Rhesus factor incompatibility.
Rh-attribution is determined in several ways. It depends on whether there is a special laboratory equipment. In his absence, rapid methods for determining the Rh factor:
- using a universal reagent;the test tube does not heat up
- on a white flat plate without heating the test tube
Determine the Rh component of fresh, non-curdled blood. It is taken from the finger or from the vein

For the express method, use universal serum, which is suitable for all blood groups. Serum is prepared by a special method. It is used in carrying out procedures for immunization of pregnant women. Bonding of erythrocytes in a test tube suggests that there is Rh-antigen in the blood.
Blood Group Compatibility Chart
The mother's body with negative rhesus perceives a fetus that inherited a positive rhesus of the father, as an alien. As a result, antibodies are produced that attack and destroy the fetus.
Sometimes this affects the development, normal growth of the baby. But serious consequences are also possible: present antigens in the blood can cause fetal death in the womb, miscarriage

Symptoms of rhesus conflict
The woman herself can not determine for herself how she feels about the development of Rhesus-conflict. The main feature is the presence in her blood of antibodies
- the fetus develops a hemolytic disease that is manifested by anemia, a violation of the internal organs of the
- in the baby is jaundice
- there is a risk of fatal hypoxic brain and heart damage
Cause of the rhesus conflict:
- caesarean section
- various complications, bleeding before or in the processchildbirth caused by placental disorders or its detachment
- , carrying out various procedures such as chorionic biopsy, cordocentesis or amniocentesis of
- and preeclampsia, diabetes, after suffering a flu or acute respiratory disease
- after intrauterine sensitization

woman expectant mother is at risk of developing Rh conflict with complications during pregnancy( toxicosis, jumps in blood pressure, infectious diseases).Possible sensitization is learned after the woman passes all the tests and the rhesus-belonging of the future parents and their blood groups is determined.
. Blood test for the Rh factor.
. It is impossible to find out independently that the pair is not suitable for each other by blood. But if a woman does not become pregnant for a long time from a partner, or if miscarriages become pregnant, doctors should be contacted for help. The "infertile" couple, having passed all the necessary tests and following the recommendations, will be able to conceive the baby, and the woman - to successfully take it out.

The first stage of the examination of the pregnant woman for the presence of antigens is the determination of Rh-affiliation of future parents. To conduct such diagnostics is recommended before conception, or at the beginning of pregnancy. With negative rhesus of both partners, further investigation is not carried out, since the conflict is excluded.
Important: if the patient's pregnancy has ended with miscarriage or abortion took place, the fetus died still in the womb or if the child was born with a hemolytic disease, then there is a big risk of a rhesus-conflict

. To know if the fetus suffers from a lack of oxygen in the Rhesus conflict, it is necessary to regularly undergo ultrasound diagnosis. Ultrasound is prescribed at the end of the 20th week of pregnancy and ending with the 36th week. The last time an ultrasound is prescribed before childbirth. This allows you to observe the growth and development of the baby.
Fetal development is also judged by examining amniotic fluid( amniocentesis) and examining cord blood( cordocentesis).Diagnosis of this type is carried out in the last trimester of pregnancy. Analysis of umbilical cord blood, how much anemia develops in hemoglobin, bilirubin, and other parameters.
What are antibodies?
In the body of a pregnant woman, the compounds of the protein structure - Rh-antibody - begin to be produced only by 7-8 weeks. Until then, there are no Rhesus antibodies in the mother's bloodstream that can harm the fetus.
For the first pregnancy is characterized by the production of large antibodies. They are not easy to penetrate the placenta to the fetus. But in subsequent pregnancies, the production of other antibodies against the Rhesus factor occurs.
Antibodies are less, but their presence is more destructive for a child, since it is easier for them to pass through the placenta and they are more aggressive. Therefore, the female immune system responds during the subsequent fetation of the fetus to the Rh-antigen faster and stronger.
Rhesus conflict in second and subsequent pregnancies
If a woman first has a baby, then the incompatibility of the blood groups of future parents will not cause a rhesus-conflict, since the amount of antibodies produced is insignificant.
The second pregnancy increases the risk of conflict. This means that at the time of birth, umbilical cord blood enters the mother's blood with protective antibodies - "memory cells".Thus, the mother's body becomes susceptible to Rh-antigen. The placental barrier of the antibody overcomes and destroys the red blood cells of the fetus.
Maximum risk for women
Mother's Rh-sensitization does not threaten anything. After a complicated pregnancy and childbirth, the mother's problems with the presence of Rh-conflict are being exhausted. But the resulting immunization may affect the recurrence of the situation during subsequent pregnancy.
Consequences of rhesus conflict for fetus
The child develops hemolytic disease in case of Rh-conflict, edema, icterus, spleen, liver increase. The blood increases the bilirubin, which poisons a small organism. A favorable prognosis: a child who is born has a high probability of developing hemolytic anemia in mild form. There is no jaundice and dropsy.
In more severe forms, hemolytic anemia with jaundice occurs. But the most serious form of the disease is exacerbated by jaundice and dropsy. A child may die in the womb
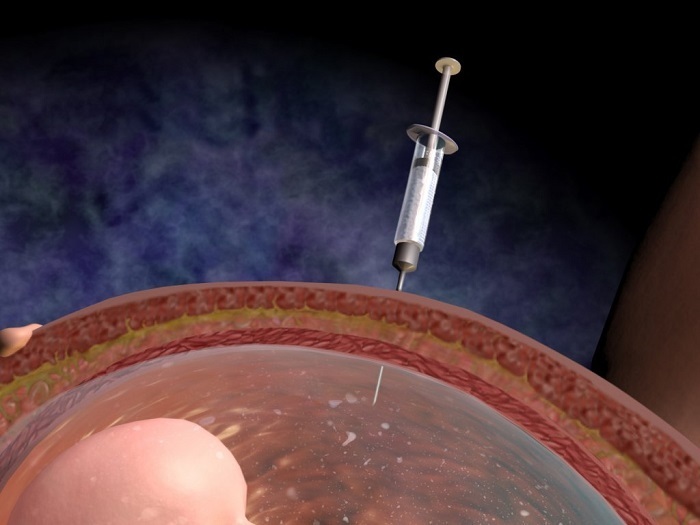
Rhesus treatment
Doctors may decide to have an intrauterine blood transfusion to a child up to 34 weeks of gestation, which improves the fetus. Transfusion is carried out through the umbilical cord. Thus, it is possible to avoid the development of anemia in the fetus.
In especially severe cases, a decision is made to stimulate preterm labor. The born child is treated for jaundice, a course of phototherapy( with the laying out under special blue lamps).You may need to repeat blood transfusion. In some cases, treatment is not required at all.

