 Genetic thrombophilia is a hereditary condition of the body in which the has a tendency to form clots of ( blood clots) for a long period of time( month, year, or lifetime) or to spread thrombus far beyond the damage.
Genetic thrombophilia is a hereditary condition of the body in which the has a tendency to form clots of ( blood clots) for a long period of time( month, year, or lifetime) or to spread thrombus far beyond the damage.
The term "thrombophilia" usually means a genetically conditioned condition, but the existence of acquired states of increased propensity to form clots often misleads people.
These states are not relevant to this concept. You can not put the equal sign between thrombophilia and thrombosis, since the genetic predisposition to thrombophilia is not necessarily realized as a thrombosis.
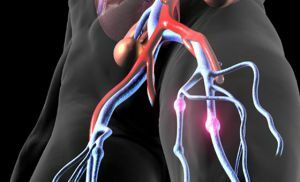
The manifestations of thrombophilia are associated with the formation of thrombi. This is due to a change in the ratio between coagulating and anticoagulating factors of the circulatory system.
With the normal blood clotting process necessary to stop bleeding, the
forms a blood clot, , which closes the vessel at the site of injury. For the implementation of the formation of a clot, certain active substances, the so-called clotting factors, are responsible.To prevent excessive blood clotting, anticoagulants exist.
That is, there is either a decrease in the number of anticoagulant factors, or an increase in the number of coagulation factors. This is the reason for the formation of thrombi, which disrupt the blood supply of tissues and organs.
Contents
- Genetic factors of thrombophilia
- Classification of the disease
- Clinical manifestations
- Diagnosis
- Genetic thrombophilia and pregnancy
- Treatment procedures
- Preventative measures
Genetic factors of thrombophilia
Genetic thrombophilia is due to a hereditary predisposition of a person. 
Therefore, there are no specific reasons for this state. There are only some risk factors that can trigger the development of this condition.
It is believed that more often thrombophilia occurs:
- in males;
- in people over 60 years of age;
- in people whose relatives suffered from thrombophilia;
- in pregnant women, in women who use oral contraceptives;
- in people with oncological pathology, with autoimmune and metabolic diseases;
- in people who have recently undergone severe infections, injuries and surgeries.
Classification of the disease
There are two main types of thrombophilia:
- Congenital( hereditary, primary) thrombophilia.
- Acquired thrombophilia.
The first type of thrombophilia is caused by anomalies in the genes that carry information about proteins involved in blood coagulation.
Among them, the most common are:
- deficiency of proteins C and S;
- deficiency of antithrombin III;
- abnormality V of the clotting factor( Leyden mutation);
- anomaly of prothrombin G 202110A.
All these congenital disorders lead to a clotting disorder.
 It is necessary to know this before making ultrasound of the veins of the lower extremities - indications and contraindications, pluses and minuses, decoding of the results.
It is necessary to know this before making ultrasound of the veins of the lower extremities - indications and contraindications, pluses and minuses, decoding of the results.
What medical rationale has sclerotherapy for hemorrhoids you can learn by studying our research on this topic.
The second type of thrombophilia occurs due to other diseases or medication. These are:
- Antiphospholipid syndrome. Characterized by the formation of excessive amounts of antibodies that destroy phospholipids. Phospholipids are important components of membranes of nerve cells, vascular wall cells and platelets. When these cells are destroyed, active substances are released that disrupt the normal interaction between coagulating and anticoagulating blood systems. As a consequence, coagulability increases, and the tendency to thrombosis increases.
- Myeloproliferative diseases. These diseases are characterized by the production of excess blood cells by the bone marrow. In connection with this, the viscosity of the blood increases and there is a disturbance of blood flow in the vessels. It also helps increase thrombogenesis.
- Acquired deficiency of antithrombin III. Characterized by a violation of the synthesis of this factor or its excessive destruction.
- Diseases accompanied by vascular damage. For example, it is known that in diabetes mellitus, the level of insulin hormone that utilizes glucose decreases, resulting in an increase in blood glucose levels. A glucose has a toxic effect on the cells of the walls of blood vessels. Damage to the cells of the vessel wall in turn provokes the release of clotting factors, a violation of blood flow and excessive thrombus formation.
Clinical manifestations of
 Often, people suffering from thrombophilia do not make any complaints and do not notice any changes in their health.
Often, people suffering from thrombophilia do not make any complaints and do not notice any changes in their health.
This is due to the fact that this pathology is characterized by a prolonged course and smoothness of the increase in clinical manifestations.
Sometimes, genetic thrombophilia manifests its symptoms several years after genetic markers of thrombophilia have been identified.
Only in the formation of a thrombus in patients there is a clinical symptomatology. The degree of manifestation of symptoms is determined by the location of the thrombus and the degree of obstruction of the lumen of the vessel:
- When blood clots appear in the arterial blood vessels, arterial thrombosis may occur. Against this background, development of ischemic stroke and attacks of acute coronary insufficiency in young people is possible. In the case of a thrombus in the placental vessels, miscarriages and fetal death in utero are possible.
- With venous thrombosis of the lower limbs, a wide range of clinical manifestations arise. There is a feeling of heaviness in the legs, a painful pain in the shin area, marked swelling of the lower extremities and trophic changes in the skin.
- With , thrombus localization in the mesenteric vessels gives rise to acute dagger pain, nausea, vomiting and loosening of the stool.
- For , thrombosis of the hepatic veins of is characterized by intense pain in the epigastric region, indomitable vomiting, edema of the lower extremities, and enlarged abdomen.
Diagnosis of
A blood test for genetic thrombophilia is the main diagnostic method.
Study of blood for thrombophilia occurs in two stages:
- on the of the first stage, the pathology is detected in a specific link of the blood coagulation system by means of nonspecific blood tests;
- on the second pathology stage is differentiated and concretized using specific assays.
In the general analysis of blood in thrombophilia, an increase in the number of erythrocytes and platelets is noted, the ratio of the volume of erythrocytes to the total volume of blood increases.
Determine the level of the D-dimer in the blood. This substance is a product of thrombus destruction. With thrombophilia, there is an increase in its number.
Assaying the activated partial thromboplastin time( APTT), mimics the natural clotting of blood and allows the to assess the degree of activity of coagulation factors .
Thrombophilia is characterized by an decrease in APTT. The level of antithrombin III, a substance that activates the anticoagulant system of blood, will be reduced. When thrombophilia is also determined by the time of clot formation in the blood plasma - thrombin time. It is decreasing.
Fibrinogen is one of the main elements of a blood coagulation system. 
With thrombophilia, its level increases. Evaluation of the clotting rate is carried out using the prothrombin index. His level will be increased.
To specific studies that allow differentiating thrombophilia with other diseases, are:
- Determination of the level of lupous anticoagulant, of a specific protein that destroys elements of vascular cell membranes. Its level can be increased in autoimmune diseases.
- Determination of anti-phospholipid antibodies , destroying cell membranes. An increase in their level may be an indicator of antiphospholipid syndrome.
- Determination of homocysteine level .An increase in its level may indicate a deficiency of B vitamins, smoking and a sedentary lifestyle.
- Genetic studies of .Allow to identify abnormalities in the genes of clotting factors and prothrombin.
All these studies in total allow you to get a genetic passport for thrombophilia.
Genetic thrombophilia and pregnancy
Many women with a tendency to increased thrombosis can tolerate a healthy child without problems.
However, there is an risk of various complications of during pregnancy.
This is due to the fact that during pregnancy, serious compensatory changes occur in the mother's body, one of which is a change in the blood coagulation system, which helps to reduce blood loss during childbirth.
Treatment procedures
In the treatment of patients with thrombophilia, specialists from various fields of medicine take part.
 For example, the hematologist studies and corrects changes in the blood composition, the phlebologist treats phlebothrombosis and thrombophlebitis, and if ineffective conservative therapy, vascular surgeons are involved.
For example, the hematologist studies and corrects changes in the blood composition, the phlebologist treats phlebothrombosis and thrombophlebitis, and if ineffective conservative therapy, vascular surgeons are involved.
Treatment of patients with thrombophilia must necessarily be comprehensive and individual .All patients undergo a generally accepted scheme for the treatment of thromboses using therapeutic and prophylactic doses.
Thrombophilia has no specific treatment, and is treated similarly to thrombosis.
Preventive measures
Specific prophylaxis of thrombophilia does not exist. A very important aspect is the prevention of thrombosis in patients with thrombophilia.
Prevention of such manifestations of thrombophilia as deep vein thrombosis, pulmonary embolism is the main point in the prevention of of this pathology.
