Content
- 1 Causes of the disease
- 2 Signs of vulvitis in women
- 3 Classification and stages of development
- 4 Complications of vulvitis
- 5 Diagnosis of vulvitis
-
6 How is vulvitis treated in adults
- 6.1 Diet and treatment regimen
- 6.2 Candles for the treatment of vulvitis in women
- 6.3 Ointments for the treatment of vulvitis in women
- 6.4 Pills for vulvitis in women
- 6.5 Hygiene procedures
- 6.6 Treatment of vulvitis in women with folk remedies
- 6.7 General recommendations
- 7 Causes and treatment of chronic vulvitis
- 8 Disease prevention
- 9 Conclusion
- 10 Reviews on the treatment of vulvitis in women
Vulvitis is a gynecological disease that can manifest itself at any age, even from the first years of life. Distinguished by unpleasant signs that cause severe discomfort. Symptoms and treatment of vulvitis in women are quite common in gynecological practice and require mandatory medical intervention.
Causes of the disease
According to the causes of vulvitis, it is customary to divide into two types:
- Primary vulvitis. This variant of the disease is caused by improper intimate hygiene or its absence. In addition, injuries and burns of the inguinal region, malfunctions of the endocrine system, allergic manifestations to cosmetics and chronic cystitis contribute to it. Less often, acute vulvitis in women, manifested by pronounced symptoms and requiring treatment, occurs against the background of long-term use of antibiotics and hormonal drugs.
- Secondary vulvitis. Caused by any external changes in the internal genital organs. Provocateurs in this case are herpes, vaginitis and other pathological processes that require treatment.
Important! One of the important reasons that often causes the appearance of vulvitis in women after 45 years is a decrease in immunity caused by a bacterial or viral disease of a systemic nature. Additional risks are created by a lack of vitamins, as well as the presence of bad habits.
Often, a decrease in immunity leading to vulvitis is caused by long-term use of glucocorticoids.
Additional factors contributing to the development of vulvitis in women at any age:
- trauma to the groin, especially scratches and scratches;
- diaper rash caused by the peculiarities of the constitution of a woman, for example, the presence of folds;
- diseases of a dermatological nature in the groin area - eczema, psoriasis, etc.;
- an allergic reaction to intimate hygiene products, including washing gels and pads;
- incorrect intimate hygiene, which leads to the need for treatment;
- tight synthetic underwear, leading to an allergic reaction;
- non-compliance with the rules for replacing tampons and sanitary pads during menstrual bleeding.
The risk of developing vulvitis is especially high if there are concomitant diseases of the endocrine and reproductive systems. They also require timely treatment.
Signs of vulvitis in women
In order to correctly diagnose the disease, it is necessary to understand what vulvitis looks like in women. Like many diagnoses, this pathology can be both acute and chronic. The second form, as a rule, is a consequence of the untreated first and is almost asymptomatic except for the period of relapses.
Characteristic signs of acute vulvitis in women:
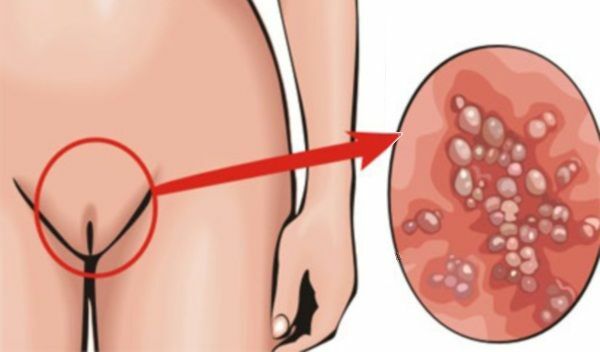
- Puffiness and hyperemia of the surface of the external labia, clitoris. The appearance of sores and pronounced erosions on them. Additionally, the inner thigh and folds of the inguinal zone may be affected.
- Soreness in the groin, which is acute on movement and urination. Itching and burning even at rest.
- Palpation of the lymph nodes located in the inguinal zone, speaks of their obvious increase.
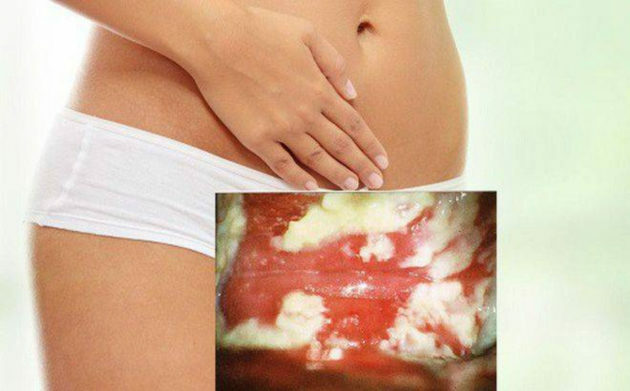
- Serous-purulent discharge, which may be interspersed with ichor. May differ, depending on the accession of a secondary infection. For example, in the presence of the Candida fungus, the discharge acquires a curdled consistency. Putrid odor of discharge.
With the progression of the pathology, there is a risk of developing diseases of the genital area, which is accompanied by the following symptoms:
- fever - with ascending infection;
- purulent discharge - with colpitis;
- cramps when urinating - with cystitis.
If the treatment of vulvitis in women is not started in time, choosing the right treatment regimen, the pathology flows into a chronic form. It is expressed by redness and soreness, moderate swelling of the inguinal zone, slight discharge, burning and itching.
Warning! Complications of vulvitis in women can lead to deformation of the surface of the genital organs and even to the fusion of the outer and inner lips. This violates not only the opportunity to lead an intimate life, but also destroys the reproductive function.
Classification and stages of development
In addition to the nature of the course of the disease, vulvitis can be classified according to the reasons that caused it. There are the following forms of pathology:
- Atopic form of vulvitis. It is a specific reaction to any irritant that has entered the external genitalia of a woman. In fact, this is an allergic response of the body.
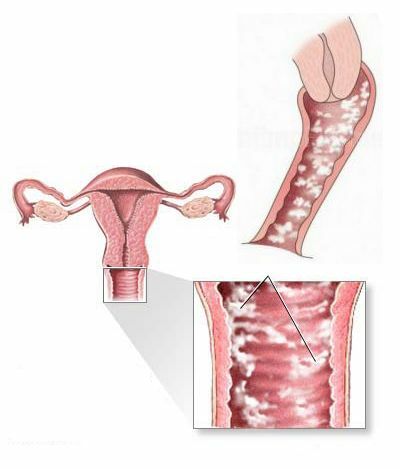
- Candidiasis form of vulvitis. Becomes a consequence of the active reproduction of the fungus of the genus Candida.
- Atrophic form of vulvitis. Most often occurs in old age or with diagnosed diabetes mellitus, when there is a structural violation of the mucous membrane.
According to the classical division of the currents, vulvitis in women can be:
- sharp;
- subacute;
- chronic;
- abscess and ulcerative condition of the vulva.
Abscesses and ulcers - an extreme degree of damage to the vulva in women
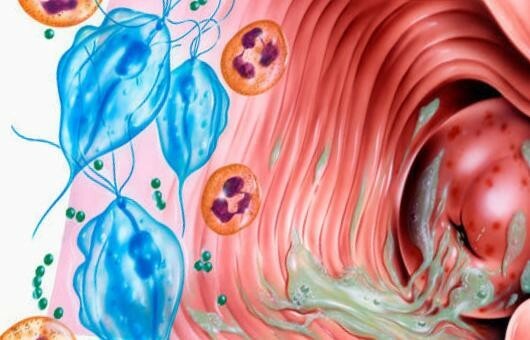
Infectious vulvitis is subject to the following classification:
- Non-specific - bacterial, which are caused by conditionally pathogenic microflora.
- Specific - as a rule, it is gonorrheal, trichomonas, mycotic, syphilitic, etc.
There are also non-tumor skin lesions of a dystrophic nature, they also affect the mucous membranes. For example, it is lichen sclerosing, leukoplakia, dermatoses and their mixed forms.
Complications of vulvitis
Since vulvitis is a diagnosis that is caused by a specific pathogen or infection, the nature of the complications of the disease depends on the type of the latter. In the bacterial form, the following negative outcomes are characteristic:
- Difficulties during pregnancy, intrauterine fetal death, miscarriage.
- Septic complications following childbirth or surgery.
- Infertility, unsuccessful IVF attempts, which are caused by inflammatory processes in the organs of the reproductive system.
- Increased risk of carrying infections that are sexually transmitted. At the same time, the mucous membrane of a woman becomes more susceptible to receiving a virus, including HIV, this is caused by a change in the pH level.
- The risk of developing cancer of the vulva and cervix increases.
In the case of an aerobic type of disease, the risk of inflammation of the pelvic organs increases. There is also an increased risk of cervical dysplasia, missed pregnancies and miscarriages.
Warning! With vulvitis in women, the disease often involves the rest of the pelvic organs, including the urinary system, in the pathological process.
Diagnosis of vulvitis
It is possible to cure a woman's vulvitis subject to correct diagnosis, during which it is possible to identify the true cause of the pathology.
Main research methods:
- Microscopic analysis of a smear from the cervical canal. Allows you to determine the type of exciter.
- Tank culture, which allows you to determine the sensitivity of the identified pathogen to antibacterial drugs.
- pH test performed with litmus papers. With the help of this study, imbalance can be identified.
An additional mandatory research method that will allow you to quickly determine the pathogen's DNA is PCR. With its help, femoflor and florocenosis are performed. Through this study, both specific infectious microflora and non-specific are revealed.
Warning! Often, with nonspecific vulvitis, a cytology test is performed, which will determine the presence of cancer cells and prevent their active development.
According to indications, it is possible to carry out additional diagnostic methods, including vulvoscopy, biopsy, histology, etc.
How is vulvitis treated in adults
The success of the treatment of vulvitis directly depends on the correct diagnosis and identification of the pathogen or other cause that led to the disease. Therapy is prescribed only after receiving the results of the studies.
Diet and treatment regimen
With diagnosed allergic-type vulvitis, compliance with the treatment regimen and compliance with food restrictions is required. The diet provides for the rejection of:
- sweets;
- spicy food;
- excess salt and smoked meats.
Additionally, therapy with the use of antihistamines is required.
Candles for the treatment of vulvitis in women
In order to level the changes at the microbiological level and restore the normal acidity of the vagina, effective suppositories are used for vulvitis in women. As a rule, they contain estriol, which eliminates dryness and itching in the vagina. This component is considered one of the safest, since it does not affect the mammary glands and endometrium in general.
Common suppositories from vulvitis for women, which are relatively inexpensive:
-
Ovestin;

In addition to suppositories, Ovestin is also available as a cream.
-
Estriol;

Estriol is a more affordable analogue of Ovestin
-
Ovipol Clio;

Ovipol Clio relieves unpleasant symptoms from the first application
Ointments for the treatment of vulvitis in women
Another type of medicine used in the treatment of vulvitis in women is special ointments for local use. For this purpose, agents with healing compounds are usually used, which give elasticity to the skin and mucous membranes, - hydrocortisone ointment, Inflorax, nystatin ointment, Radevit, tetracycline ointment, Actovegin, Levomekol, etc. d.

Hydrocortisone ointment can be applied directly to the mucous membrane
Pills for vulvitis in women
In addition to local treatment, with vulvitis in women, the use of antibiotics is indicated, the name and group of which depends on the type of pathogen. The use of broad-spectrum drugs is practiced. To determine the group that will achieve the desired effect, will allow a preliminary analysis for bacterial culture, which determines the sensitivity of pathogens.
Important! With an allergic type of vulvitis, antihistamines are required.
Hygiene procedures
Successful therapy for vulvitis in women is possible with a combination of drugs in compliance with the rules of hygiene. It is necessary to use only neutral products and wear natural underwear that does not cause unnecessary friction, which leads to irritation.
Treatment of vulvitis in women with folk remedies
Traditional medicine recipes will make it possible to achieve some progress in the treatment of:
- Mix aloe juice with any vegetable oil and apply to the affected areas.
- Lubricate the mucous membrane with sea buckthorn oil.
Additionally, it is recommended to take decoctions of herbs that have a sedative effect, which is necessary in the treatment of vulvitis in women.
Attempts to treat vulvitis only with folk remedies will not bring results, but will only lead to the formation of a chronic form
General recommendations
General clinical guidelines regarding the treatment of vulvitis in women indicate the need for an integrated approach. The right choice of antibiotics should be combined with local preparations and means to raise immunity.
Causes and treatment of chronic vulvitis
The main cause of chronic vulvitis is the acute form that has not been fully cured. Treatment of this type is systemic, it requires regular monitoring and testing. Often, the remission of the symptomatic picture of vulvitis in women does not mean recovery.
Important! To check whether the pathogen that caused vulvitis in a woman has left the body is possible only with the help of laboratory tests.
When treating the chronic form of vulvitis in women, the doctor selects the treatment regimen individually, trying a combination of different drugs.
Disease prevention
The basis for the prevention of vulvitis in women is the timely detection and elimination of any pathogens that cause diseases of the genitourinary system. Additional measures:
- Examination and treatment of the sexual partner in diagnosed vulvitis in a woman.
- The use of barrier contraception, the rejection of casual intimate relationships, leading to the development of infectious vulvitis in women.
- Compliance with the rules of hygiene and sanitary standards, the absence of which often causes vulvitis in women.
In fact, the prevention of vulvitis in women is similar to any infectious disease, especially if it is caused by the activity of pathogens.
Conclusion
Symptoms and treatment of vulvitis in women require mandatory medical attention, only a doctor can prescribe a competent treatment regimen, especially if there is a chronic form. The key to recovery will be the correct diagnosis and identification of the trigger that gave impetus to the development of the disease.
Reviews on the treatment of vulvitis in women
Marina Kolosova, Moscow
She treated vulvitis in an acute form, which arose against the background of a common thrush. I did not even expect that a simple candida would give such an effect. In addition to suppositories and antifungal drugs, the doctor prescribed antibiotics. Itching and discomfort, characteristic of vulvitis, did not disappear immediately. Condition is not pleasant!
Elena Petrova, Stavropol
I didn’t even expect that I was sick with something, I attributed the burning sensation and periodic discomfort to age-related changes. Turned out to be chronic vulvitis. They ran all the tests, they even did a biopsy, but there is no activity of cancer cells. Now at the stage of treatment of vulvitis with suppositories and antibiotics.
The information and materials on this site are provided for informational purposes only. You should not rely on the information as a substitute for actual professional medical advice, assistance or treatment.
