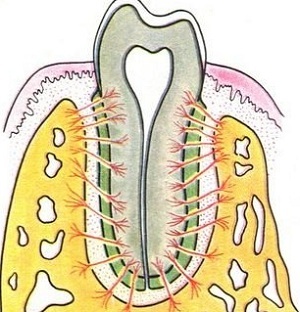
 Periodontium( perecenter) - a binder that holds the tooth in the bone, it is represented by a dense formed connective tissue, due to which a special type of articulation of the teeth with the tissues of the jaw is formed.
Periodontium( perecenter) - a binder that holds the tooth in the bone, it is represented by a dense formed connective tissue, due to which a special type of articulation of the teeth with the tissues of the jaw is formed.
The tooth surface, the periosteum of the alveoli and periodontium form the so-called."Pinned" type of joint articulation( Latin gomphosis).
Contents
- Anatomical features
- Functional load
- What diseases are affected?
- Different forms of periodontitis
- Development of periodontitis
- In dry residue
Anatomical features of
Periodontitis is a bundle with a thickness of about 0.2 mm. The periodontal ligament is a tightly formed connective tissue, most of which is made up of 2-A type collagen fibers. The peculiarity of them is that they have a shape resembling a spring. Due to this, the fabric represented by these fibers is strong( in contrast to those where the fragile elastin fibers predominate), but at the same time has the ability to slightly stretch.
The fibers themselves at the attachment site are divided into:
- alveolar;
- oblique;
- apical( apical);
- horizontal;
- are intraradicular( inter-root).

In addition to the organized bundles of collagen fibers, peri-cement consists of typical cellular elements:
- connective tissue cells : fibroblasts and fibroblasts - the latter produce collagen fibers;
- cells of the immune system - macrophages( tissue immunity, APC), lymphocytes and neutrophils( in the presence of foci of infection come out of the bloodstream);
- epitheliocytes of the Malassé islets are rudimentary accumulations of epithelial cells remaining after the formation of the Gertvig vagina.
Nutrition and innervation of the periodontal tissues of the tooth are carried out:
- by the blood vessels , originating from the upper anterior, middle and posterior alveolar arteries of the upper jaw, and from the lower alveolar artery on the lower jaw;vessels originate from the alveolar branches of the arteries( r. alveolares);
- nerve fibers , providing proprioceptive innervation, they belong to the parasympathetic autonomic nervous system and carry out reception due to the glomerular and bushy nerve endings that make up the fleshy nerve fibers;
- lymphatic drainage is performed on the course of venous vessels pericsement.
Functional load
Periodontal functions are as follows:
- Supporting bearing .The tissue takes part in the attachment of the tooth to the alveolar part of the jaw, provides an even transfer of the masticatory load to the bone tissue.

- The depreciating is provided by the structure of collagen fibers. Their ability to elastic stretching helps to reduce the masticatory pressure on the periosteum of the alveoli( according to various studies, the strength of the masticatory load reaches 100 to 200 kg).
- Reflex - periodontium takes part in regulating the strength of the masticatory pressure due to the presence of nerve endings in it( afferent link).
- Trophic is carried out due to the neurovascular bundle, which is part of the tissue.
- Barrier is realized with the help of local immunity factors( macrophages and antigen-presenting cells in the periodontal composition), as well as plasmocytes, leukocytes and lymphocyte infiltration of tissues.
- Sensory - nociceptive innervation responds to inflammatory changes in both the periodontal and alveolar parts of the bone, which forms human behavior, aimed at getting rid of pain and prevents the spread of infection.
- Participation in teething and growth of jaw bones - physiological load on bone tissue, which is formed with the participation of periodontal, stimulates the development of the dentoalveolar system. Clinically found that children who are lazy to chew solid food, the timing of teething changes for 2-3 months. Also, the lack of masticatory load in childhood leads to micrognathia and microgenia, which, when a permanent bite is developed, leads to multiple orthodontic pathologies. Chewing load, realized through periodontium, contributes to the osteoplastic processes of the alveolar part of the jaw bones.
What diseases are affected?
Periodontal tissues are prone to dangerous diseases, the development of which can lose their teeth.
Different forms of periodontitis
Periodontitis is one of the complications of tooth decay, in which the tooth pulp is first infected when it is connected to a carious cavity, and then it dies off the pathogenic microflora reaches the periodontal period. Periodontitis is divided into acute, chronic and exacerbation of chronic form.
Acute periodontitis is distinguished by the type of exudate:
- serous form;
- purulent form.

Chronic periodontitis differs according to what pathological formation is formed in the productive phase of inflammation:
- Fibrous appears on the roentgenogram as a slight extension of periodontal disease. From the point of view of histology - in the apical part of the root of the tooth appears a scar( friable unformed connective tissue).
- Chronic granulating - at the tip of the root radiographically determined bone loss without clear boundaries( the so-called "tongues of flame").It is an inflammatory destruction of the bone of the alveolus with the formation in its place of immature scar tissue( granulations).
- Chronic granulomatous is characterized by the appearance of cysts in the apex region of the affected tooth. The X-ray picture reveals a focus with clear boundaries, which most often has a spherical shape.
Acute forms and relapses of the disease provoke such symptoms:
- intensifying during chewing aching permanent pain in the tooth;

- redness and swelling of the mucosa in the projection of the apex of the root of the tooth or the entire root;
- percussion is sharply painful;
- a large carious cavity( the crown can be almost completely destroyed), which communicates with the pulp chamber of the tooth and is painless when probing;
- preventive preparation is painless.
Distinguishing Symptoms of Chronic Form:
- transition from a cold to a warm room provokes a aching pain in the tooth;
- feeling of heaviness and discomfort in the tooth;
- soreness with pressure on the tooth and chewing;
- fistula in the apex projection area( with a granulating form);
- darkening of the crown;
- a large carious cavity that communicates with the pulp chamber and is painless when probing;
- percussion gives a weak pain.
Development of periodontitis
It is an inflammatory disease of all tissues that surround the tooth. Since the periodontium is part of the periodontal disease, it also becomes involved in the inflammatory reaction.
In dry residue
Periodontium is a ligament that has a unique structure and participates in the formation of bone articulation, which has no analogues in the  organism. Despite the small thickness, the ligament is able to withstand large gum loads and gently distribute the chewing pressure on the bone.
organism. Despite the small thickness, the ligament is able to withstand large gum loads and gently distribute the chewing pressure on the bone.
In the absence of timely treatment of caries, the inflammatory focus in periodontium can become a hotbed of chronic infection of the body( chroniosepsis).
This is a predisposing factor for the development of low immune reactivity and the distortion of the immune response( sensitization with microbial antigens can trigger allergization, or in combination with minor traumas lead to aseptic inflammation( the theory of the appearance of osteomyelitis according to Lukomsky)
