The inevitable changes that are characteristic of menopause, find response in different parts of the body. One of the features of the new condition is a decrease in the activity of immunity. This cause, as well as others, causes the onset and unexpected development of diseases.
Even gynecological ailments, which seemingly should give a woman a break from their presence, are able to intensify, threatening to move to a more serious stage. Hyperplasia of the endometrium in menopause is no exception. It can show up for the first time, without showing any noticeable signs, to quiet down or to remind oneself with renewed vigor.
What does "hyperplasia" mean?
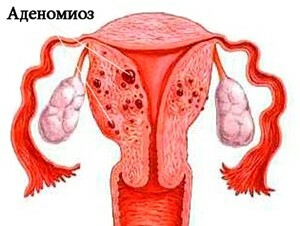 The uterus has a mucosal coating called the endometrium. This body consists of several layers, each has its own functions. Endometrium is not the only part of the uterus, with its other departments it has clear distinctions. But for many reasons, to identify which is reliably difficult, its cells begin to germinate into the muscular layer of the organ.
The uterus has a mucosal coating called the endometrium. This body consists of several layers, each has its own functions. Endometrium is not the only part of the uterus, with its other departments it has clear distinctions. But for many reasons, to identify which is reliably difficult, its cells begin to germinate into the muscular layer of the organ.
The thickness of the mucosa increases, causing hormonal, endocrine and reproductive disorders. Hyperplasia of the endometrium in menopause is its anomalous spread into the layers of the uterus. Still it is called adenomyosis. Depending on which mucosal cells predominate in abnormal formations, not one type of disease is distinguished.
The harbinger of adenomyosis is endometrial hypertrophy in menopause. This is the growth of the volume and mass of the layers of the uterine mucosa. When menstruation is still coming, at the beginning of the period this is normal, since in the end it will decrease, and the upper layer will be rejected. But in postmenopause, this is an alarming sign, since the thickness of the endometrium remains constant in the norm, having definite values. Following the growth of volumes, an increase in the number of cells of the organ may begin.
What is adenomyosis?
Despite the fineness of the endometrium, it includes a different kind of cells. The tissues found in the thickness of the myometrium may be a cluster of one or several types. This, as well as the location of abnormal growth, determines the type of disease. Specialists call the following forms of hyperplasia:
- Glandular;
- : Glandular cystic;
- Focal;
- Atypical.
Glandular cystic and cystic disease
 The glandular cystic endometrial hyperplasia in menopause appears most often due to age-related causes. This hormonal failure, its risk with menopause has natural causes. Diabetes mellitus, benign tumors in the mammary glands, obesity, thyroid problems, often observed in women after 45, are favorable for the development of the ailment circumstances.
The glandular cystic endometrial hyperplasia in menopause appears most often due to age-related causes. This hormonal failure, its risk with menopause has natural causes. Diabetes mellitus, benign tumors in the mammary glands, obesity, thyroid problems, often observed in women after 45, are favorable for the development of the ailment circumstances.
This type of adenomyosis is distinguished by the fact that its basis is glandular tissue, but the growth is supplemented by the formation of cysts and nodules in it. The latter may also be found on the ovaries. Cells of the mucous membrane seep into the mouth of the glands, clogging them and putting an obstacle to the outflow of their contents. Cavities filled with mucus grow.
Cystic endometrial hyperplasia in menopause is threatened by the fact that benign formations can degenerate into a tumor. It is formed a little differently than glandular, although changes exist in the same tissue. Cysts with this form of adenomyosis are formed by increasing the size of the glands.
Focal hyperplasia
The forms of malaise described above are a uniform penetration of endometrial tissue into the muscular layer of the uterus. But it happens that it reveals pathological areas of limited size. This is focal hyperplasia.
It is predominantly connective tissue, not glandular. It can also be collected in polyps, having the appearance of rounded formations on the foot with a shiny pink shell. They are in the singular and in the plural. Polyps are located more often in the upper segment of the uterus, near the fallopian tubes. They are pierced by blood vessels, which are sometimes damaged.
To the transformation into a cancerous tumor of this type, endometrial hyperplasia in postmenopause is more likely than in the earlier period.
Atypical adenomyosis
In the anomalously widened thickness of the endometrium, a special type of cell sometimes appears, called atypical cells. Most often this occurs when glandular tissue prevails over the connective. Epithelium is actively divided with the formation of papillae, excessive branching of the glands, other pathologies at the cell level.
Similar can be found throughout the entire surface of the endometrium or in individual parts of the endometrium. The latter is especially dangerous because of the high risk of transition to a malignant tumor.
Why does hyperplasia occur?
Having realized the threat that the disease brings, many will want to know why endometrial hyperplasia occurs in menopause or continues to develop. The reasons can be formed long before the onset of menopause. Among the known causes of hyperplasia:
-
 Hormonal imbalance. In menopausal age, an excessive amount of estrogens can be observed in comparison with progestins. And although all hormones are produced in a smaller amount, their confrontation does not end, but can be exacerbated by the uncontrolled use of drugs that remove menopausal syndrome. Most of them are estrogen-containing. The same role can be played by birth control pills;
Hormonal imbalance. In menopausal age, an excessive amount of estrogens can be observed in comparison with progestins. And although all hormones are produced in a smaller amount, their confrontation does not end, but can be exacerbated by the uncontrolled use of drugs that remove menopausal syndrome. Most of them are estrogen-containing. The same role can be played by birth control pills; - Metabolic metabolic abnormality. With age, he leads to the appearance of excess fat, which has the ability to produce estrogens. As a result, the balance again changes in favor of these substances, progesterone is suppressed. Exchange disturbances provoke diabetes, vascular problems, malfunctions with the liver. And this will also cause a thickening of the endometrium in menopause;
- Endocrine abnormalities. The adrenal glands, the pancreas and the thyroid gland produce hormones that affect the overall background, and consequently, the condition of the reproductive system. Failures in their work lead to an abnormal amount of estrogens, which means that it can cause adenomyosis;
- Age changes in the mucosa of the genital organs. Shells become thinner, but become more susceptible to any effect. Increased risk of inflammation, infection. In the uterine cavity and its tissues, a large number of immune components are formed, spurring the rate of multiplication of the cells of the membrane;
- Frequent invasion of the uterus. Because of them, mucosal receptors almost do not react to the effects of progesterone. And the natural for menopause ratio with estrogens does not help to protect the cells of the body from increased fission. The less a history of abortions, scraping, the better for mucosal health in menopausal age;
- Genetic predisposition. The pathology of the endometrium in menopause will most likely arise in those whose ancestors on the female line suffered from malaise;
- Immune failure. It consists in the fact that the protective components produced by the body perceive the uterine mucosa as foreign tissues. This forces the latter to intensively produce their own kind.
The appearance of adenomyosis can be prompted by the presence of fibroids, mastopathy.
Symptoms of the disease
The endometrial hyperplasia in postmenopausal symptoms shows slightly different than in young women with the same diagnosis. This is due to differences in the hormonal balance. Adenomyosis is manifested:
- Sudden bleeding, which can be of a nature of anoint or intense. They can not be confused with the monthly ones, at the described stage the function of the ovaries has finally died out. However, endometrial hyperplasia in menopause without discharge also happens;
- Pain in the abdomen, drawing character;
- Increased fatigue and irritability;
- Headaches.
Some may occasionally have a strong causeless thirst( due to jumped blood sugar), to grow weight. And sometimes the endometrial hyperplasia in menopause does not show symptoms at all, revealing itself only during routine examination. That is why it is important to monitor the condition of the reproductive organs even when their main functions have already been performed.
When do you need to worry?
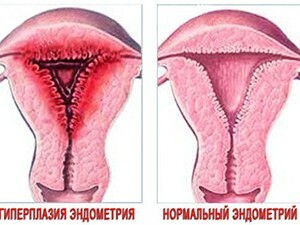
 Diagnose adenomyosis and establish its kind of specialists. To do this, hardware methods are created, the main one of which is ultrasound. It is held annually and in the absence of problems. There is such an indicator as the thickness of the endometrium, in postmenopause its norm is 4-5 mm, not more. At this stage, it atrophies, because in the mucous there are no repeated changes. It is also acceptable for the fusion of some parts of the uterus, the appearance in the cavity of the fluid due to the partial narrowing of the canal of its neck.
Diagnose adenomyosis and establish its kind of specialists. To do this, hardware methods are created, the main one of which is ultrasound. It is held annually and in the absence of problems. There is such an indicator as the thickness of the endometrium, in postmenopause its norm is 4-5 mm, not more. At this stage, it atrophies, because in the mucous there are no repeated changes. It is also acceptable for the fusion of some parts of the uterus, the appearance in the cavity of the fluid due to the partial narrowing of the canal of its neck.
The norm of the endometrium in menopause also includes the assessment of the specialist's structure. If it sees changes that do not knit with age, their character is determined.
The thickness of the endometrium with a climax of 6-7 mm is the reason for closer observation. The woman will have to do ultrasound after 3 months and in six months.
A thick endometrium in menopause is called such, starting from 8 mm. In this case, the indicator forces to scraping and analyzing the material obtained. And if it is 10-15 mm, a histological examination will be necessary.
Mucus in the uterus during uropes in menopause should be considered in conjunction with other symptoms. If there is pain and discharge with blood, it is not simply the result of natural organ atrophy, but a sign of inflammation, hypertrophic changes in the membrane.
Getting rid of adenomyosis in menopause
Treatment of endometrial hyperplasia in menopause is determined by the type and extent of the pathology, as well as the duration of the course. There are several options for eliminating, as an additional can be used and home methods.
To choose the methods of treatment should a doctor, amateur performance will lead to increased symptoms, neglect of the disease. It is dangerous for life, because some types of adenomyosis are able to transform into cancer.

Even in the absence of symptoms, it will subsequently be necessary to monitor the state of the endometrium during visits to the doctor.
Medications for adenomyosis
 Endometrial hyperplasia in menopause treatment without surgery can have only in the absence of fibrotic polyps. Drug therapy is the effect of hormonal drugs to reduce the effect on the uterine mucosa of estrogens. The following agents are used:
Endometrial hyperplasia in menopause treatment without surgery can have only in the absence of fibrotic polyps. Drug therapy is the effect of hormonal drugs to reduce the effect on the uterine mucosa of estrogens. The following agents are used:
- Megestrol acetate;
- Medroxyprogesterone;
- Hydroxyprogesterone caproate;
- Norethisterone;
- Goserelin.
- Buserelin;
- Zoladex;
- Diferelin;
- Danazol;
- Gestrinone.
Postmenopausal hyperplasia is treated with the mandatory intake of
- Ursosana, Phosphogliva, Essentiale for liver repair;
- Heparin, Hepatrombin for inhibiting blood clotting.
Gestagenes and agonists of gonadotropin-releasing hormones, like antigonadotropins, take from 3 to 6 months, constantly following ultrasound for the state of the endometrium.
Sometimes, drug therapy is used before surgery to narrow the foci of adenomyosis. Intervention in this case will be the least traumatic.
 We recommend reading an article on postmenopausal women. You will learn about the manifestations of this condition, the features of the discharge, the extinction of the reproductive function, the need for taking medications.
We recommend reading an article on postmenopausal women. You will learn about the manifestations of this condition, the features of the discharge, the extinction of the reproductive function, the need for taking medications.
When can I do without surgical treatment?
Treatment of endometrial hyperplasia in postmenopause is more often surgical, especially when it recurs, or there are prerequisites for the onset of cancer. Atypical cells found in the organ, a direct need to be operated on. Surgical intervention may be:
- In the curettage. Scraping in menopause is recommended at a 10-mm thickness of the mucosa. It is also very informative for diagnosis. The doctor removes the upper layer of the mucosa with all the growths, doing this under intravenous anesthesia. The operation lasts 20-30 minutes;
- In moxibustion. This method is suitable for focal distribution. Laser treated areas of adenomyosis. They are destroyed and taken out later on their own;
- In cryodestruction. The method is similar to cauterization, but it uses not high, but low temperatures. Pathological areas die and also leave the uterine cavity;
- In a hysterectomy. With a high risk of developing cancer, that is, complicated types of atypical hyperplasia, the uterus is removed. In late menopause, a similar threat can hang over the ovaries. And because at this age, the operation also captures all the appendages of the uterus.
Will people's ways help?
Treatment of endometrial hyperplasia in postmenopausal folk remedies should not be taken as a basis. As an addition you can use:
- Mixture of the juice of burdock root and golden mustache. Take equal proportions and take 1 tablespoon.twice a day;
- Alcoholic tincture of nettle. On 200 g of grass you need 500 ml of liquid. Insist 3 weeks in the dark, drink 1 tsp.in the morning and before bedtime.
The first in the list should be regular examinations at the gynecologist, despite of excellent state of health.
