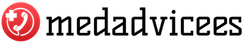
 Varicocele testis is a disease that applies exclusively to men. We are talking about blockages and widening of the venous plexuses that divert blood from the testes, appendages of the testicles and scrotum.
Varicocele testis is a disease that applies exclusively to men. We are talking about blockages and widening of the venous plexuses that divert blood from the testes, appendages of the testicles and scrotum.
These venous plexuses are located mainly behind the testicles. Each testicle has a "proper" blood supply and, consequently, varicocele, in most cases, is one-sided, much less often bilateral. More often there is a varicocele of the left testicle.
With the expansion of the venous plexuses it simultaneously reaches the hemostasis and, thus, the deterioration of the return of venous blood back to the bloodstream. As the blood entering the testicle lingers longer, it heats up, which can have a negative effect on fertility.
The fact is that spermatozoa need a colder environment for their development. Therefore, the testes are located outside the body, where the temperature is lower. Because of hemostasis, the flow of blood through the testicle also slows down and worsens its blood supply.
Contents
- What triggers the development of the disease
- Why is the left side suffering more often?
- Diagnosis of
- Diagnosis of
- Diagnosis of
- Diagnosis of
- Sonographic examination of
Doppler examination of
- Sonographic examination of
- Complex treatment of
- Surgical therapy of
- Non-surgical treatment of
- Testicular pain after surgery - causes and solution of
- For the prevention of
What causes the development of
The most common causes of the disease includeself:
- intra-ultrasound temperature increase caused by varicose veins of the venous plexus;
- reflux of adrenal metabolites( prostaglandins and catecholamines);
- dysfunction of Leydig cells;
- hypoxia due to venous stasis.
Why does the left side suffer more often?
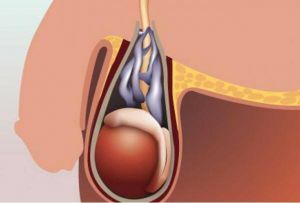
 In the majority of primary varicocele are present on the left side, in the specialized literature the assumptions are stated that this percentage reaches 78-93%.In 10% of patients bilateral varicocele was registered and only 2% had exclusively right-sided.
In the majority of primary varicocele are present on the left side, in the specialized literature the assumptions are stated that this percentage reaches 78-93%.In 10% of patients bilateral varicocele was registered and only 2% had exclusively right-sided.
In connection with third-party asymmetry, a rectangular arrangement of the left vein of the testicle is indicated with respect to the renal vein, which is more prone to reflux than the oblique location of the right-sided testicular vein relative to the inferior vena cava.
In the renal vein, there is also a significantly higher pressure than in the inferior vena cava.
Another reason that the left testicle is more often affected than the right one, can be:
- a large length of the left testicular vein( on average, 10 cm);
- , along with, on the left, about 2 times more often there is a lack or absence of venous valves( on the left they are absent in 40% of cases, on the right - only in 23% of cases);
- an important role is played by a greater number of left-sided collateral veins and a more rare lowering of the left testicle into the scrotum.
All causes can act separately or in combination.
Symptoms of the disease
Varicocele may not cause any subjective symptoms, which is why it is most often found in a general examination of the patient.
The most common manifestations are the following:
- pain in the scrotum;
- painful movement;
- bulge over the egg;
- increased temperature of the surrounding tissue.
 Pain, as a rule, is pressing, and a feeling of heaviness in the scrotum is sometimes the main reason why a person seeks medical help. However, varicocele may be completely asymptomatic cause of impaired spermatogenesis and male infertility.
Pain, as a rule, is pressing, and a feeling of heaviness in the scrotum is sometimes the main reason why a person seeks medical help. However, varicocele may be completely asymptomatic cause of impaired spermatogenesis and male infertility.
Reducing the concentration and motility of spermatozoa belongs to 65-75% of men with this disease.
Varicocele can cause hormonal deficiency in men who do not have a local( in the scrotum) symptomatology.
With prolonged development of the disease, hypoplasia or testicular hypotrophy is often observed.
Diagnostic methods
When physically examined in the standing position, you can distinguish 3 stages of the disease:
- I degree, - a small, invisible swelling at visual inspection, only visible with a Valsalva test;
- II degree, - easily perceptible swelling of the veins, or visible after the sample;
- III degree, - varicocele, visible without the use of the Valsalva technique.
Sonographic Examination
A sonographic examination carried out in a B-mode with a high-frequency ultrasound probe allows the contents of the scrotum to be displayed, the size of both testicles, their echogenicity, echostructure, width / volume of the enlarged veins and the presence of the corresponding disease.
Conducting dopplerography
This study allows to evaluate the presence of renospermatic reflux, as well as to determine its degree:
- I degree, - reflux at maximum Valsalva test, standing;
- II degree, - reflux with a minimal Valsalva test, standing;
- III degree, - reflux when carrying out the sample in prone position.
Complex treatment approach
Treatment of varicocele can be divided into non-surgical and performing the operation
Surgical therapy
Operations that are used in modern medicine for the treatment of varicocele: 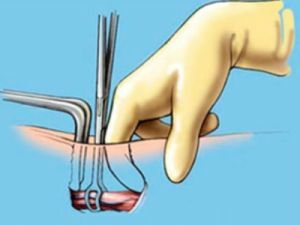
- Retroperitoneal operations .Ligation of the hollow seminal vein - Bernardi's operation -( with preservation of the testicular artery) or Palomo operation( with resection of the vascular bundle and the testicular artery).
- Inguinal operation .Seeding of the vein( or several veins) at the height of the inguinal annulus - Ivanissevich's operation - or the Amelar operation with the mobilization of the seed funnel from the inguinal canal without opening the canal.
- Operation of the scrotum .Bandaging and extirpation of the venous plexus according to Narat or Kocher.
- Laparoscopic surgery .Laparoscopic ligation of the testicular vein with or without preservation of the testicular artery( laparoscopic equivalent of surgery by Bernardi and Palomo)
- Microsurgical operations - microsurgical intervention is applied in the area of venous anastomosis between the testicular and epigastric veins or varicocelectomy.
Non-surgical methods of treatment
Non-surgical therapy includes:
- antegrade( scrotal, scrotal) sclerotherapy of the testicular vein;
- retrograde sclerotherapy of the testicular vein;
- balloon occlusion of the testicular vein;
- spiral occlusion of the testicular vein.
Also with varicocele, a very useful massage of the testicles:
Testicular pain after surgery - causes and solution
 In the field of a surgical wound, nerves pass which innervate the skin of the inguinal region. If the testicle hurts after the operation, but the varicocele does not develop again, no reoperation is performed.
In the field of a surgical wound, nerves pass which innervate the skin of the inguinal region. If the testicle hurts after the operation, but the varicocele does not develop again, no reoperation is performed.
Certainly, an ultrasonic flaw test should be performed. If visualization tests do not show complications, only symptomatic treatment with analgesics and regime adaptation are prescribed.
It should also be understood that the disease prevents proper nutrition of the testes and raises the temperature in the scrotum. The result is a deterioration in sperm production and a decrease in the secretion of male hormones.
Ultimately, these factors lead to a reduction in erection and ejaculatory failure;In addition, due to the disease, infertility may develop.
For the prevention of
If the varicocele is properly treated, the prognosis will be positive. Preventive measures that can be recommended by a physician, in  mainly, include wearing supportive underwear. In families where the disease occurs frequently, it is desirable to avoid conditions in which it comes to increasing the pressure in the abdominal cavity. These include:
mainly, include wearing supportive underwear. In families where the disease occurs frequently, it is desirable to avoid conditions in which it comes to increasing the pressure in the abdominal cavity. These include:
- chronic cough;
- constipation;
- lifting heavy items.
If there is an increase in the testes, their soreness or feeling of pressure, then it is advisable to pass the examination as soon as possible.
It is necessary to visit a urologist who, using simple and painless methods, will be able to determine what disease is taking place.