Periodontitis is an inflammation of the periodontal tissue, a connective tissue located between the alveolar plate and the root of the tooth.
Periodontitis is an inflammation of the periodontal tissue, a connective tissue located between the alveolar plate and the root of the tooth.
Granulating( granulated) periodontitis is the most active form of periodontal inflammation. Unlike more stable and asymptomatic fibrotic and granulomatous periodontitis, it develops dynamically with short periods of remission and severe exacerbations.
Inflammation is characterized by the generation of granulation tissue replacing the destroyed areas of dentin and alveoli. The focus of destruction is unstable, prone to increase. Inflammatory process extends to adjacent teeth, jaw, soft tissues of cheeks and gums, sometimes reaching the surface of the skin of the face or neck.
content
- The causes and mechanism of development
- forms of the disease: features symptomatology
- Acute for
- chronic stage
- period of remission
- Exacerbation
- The diagnosis
- Therapies
- chronic stage
- remission period
- Step exacerbation
- Surgery
- forecast and
prevention Causes anddevelopment mechanism of
The development of granular periodontitis occurs usually due to infection, trauma or unsuccessful treatment of pulpitis andcaries.
In the infectious path of development, the primary role is played by the complication of pulpitis or caries. Bacteria( streptococci, staphylococci, etc.) most often penetrate into the periodontium from the root canal with necrotic pulp. A marginal path of development of pathology is also possible: penetration of microorganisms into the periodontium through the edge of the gum and a bunch of teeth.

Simple tooth injury can cause serious complications
To traumatic periodontitis leads to physical impact on the tooth. For example, due to a shock, or in the case of an improperly installed artificial crown or seal.
The medical cause of the disease is the traumatizing of tissues with endodontic instruments or exposure to them with aggressive medicines such as arsenic paste, etc.
The development of granulating periodontitis provokes poor oral care, an incorrect bite, some diseases( diabetes, etc.).
The development of the pathological process is expressed in the proliferation of connective granulation tissue( usually at the apex of the root), destruction of the periosteum, resorption of dentin and cement of the tooth, resorption of the plates of the alveoli. With the spread of periodontitis on the soft tissues of the gums and jaw, abscesses and fistulas are formed with the release of serous-purulent contents.
In general, the development of the disease goes in the following direction:
- widening of the periodontal gap;
- formation of connective tissue in replacement of destroyed bone and tissue structures;
- formation of purulent cysts.
Forms of the disease: features of the symptomatology
According to the clinic and pathomorphology, granulating periodontitis can be:
- acute;
- chronic in remission phase;
- chronic in the phase of exacerbation.
Symptoms and clinic of granular periodontitis are determined by the form of the disease.
Acute course of
The main symptom of an acute process is prolonged localized pain, at first not very strong, then more intense, pulsating. Irradiation of pain indicates a purulent form. The acute course lasts from a few days to two weeks. Conventionally, there are 2 stages of the process:
- The first phase of the .Inflammation is characterized by prolonged aching pain, increasing when the affected tooth is pressed. Percussion fixes the increased sensitivity of periodontal disease.
- The second phase of the .Transition of the disease into the exudative stage. The spreading serous-purulent infiltrate causes swelling of soft tissues, sensitivity and an increase in regional lymph nodes. Inflammation manifests itself by strong continuous pains, pronounced soreness when the tooth is pressed. Even a slight touch with his tongue causes severe pain. There is a feeling that the tooth has moved out of the soft tissues. Percussion is extremely painful, there is an irradiation of pain. General malaise is noted, it is possible that the temperature rises to 37-38 ° C.A blood test records an increase in ESR and leukocytosis. At the same time, the radiography of changes in the periodontium does not show.
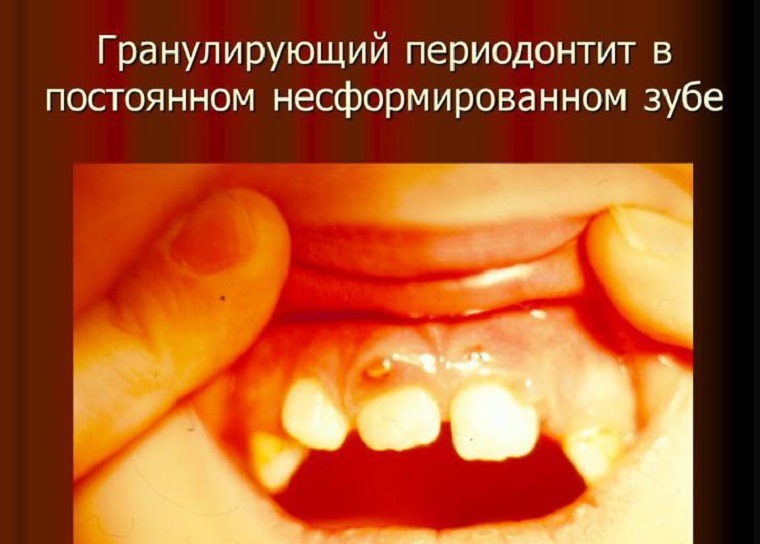
On the not formed tooth, abscess and abscess
can also occur. Chronic stage
Even in the chronic phase, the granulating periodontitis proceeds dynamically, with frequent exacerbations and short remissions.
The period of remission

In the photo, the granulating( left) and granulomatous( right) periodontitis
The disease manifests itself with occasional not very pronounced discomfort or minor pain sensations - raspiranie, weight, awkwardness. There is hyperemia and vasoparosis. Palpation and percussion are uncomfortable.
In chronic periodontitis, from time to time, pus is formed, fistulous moves occur in the adjacent soft tissues, mouth, carious cavities. It happens more often without symptoms, but only if pus has a lot to go without hindrance. If the channels overlap, for example, with food remnants or by closing the fistula itself, the pus accumulates, causes the tissue to burst and pain intensifies. With a decrease in immunity, the infection can spread further, leading to an escalation of the disease.
Exacerbation of
Exacerbations occur when the abscess capsule ruptures, prevents the removal of pus from the area of inflammation, weakening of immunity.

Periodontitis in the acute stage is often accompanied by fistula
Fistula can appear in the mouth, on the face( chin, cheeks, corners of the eyes).Exudate is released from the mouth of the fistula. Subsequently, the fistula is tightened by the scar.
Exacerbation is accompanied by a paroxysmal, intensifying with thermal and physical impact on the tooth with pain. Visually observed hyperemia, pastosity and swelling of the gums. When probing the mandibular lymph nodes from the affected teeth, their increase and a slight soreness is fixed. The patient's tooth is slightly mobile.
During an exacerbation, inflammation zones are formed, from which pathogenic bacteria and their metabolic products enter the blood, leading to sensitization of the body. With the removal of pus, intoxication is reduced, and the disease passes into an asymptomatic stage.
Corking the fistula again leads to an exacerbation and intensification of intoxication.
Diagnosis of
Differential diagnosis of granular periodontitis consists in the exclusion of granulomatous and fibrous form of the disease, actinomycosis of the face, pulpitis, jaw osteomyelitis, and circumcision cyst. The following diagnostic types are used:
- Clinical .As a rule, the examination reveals a broken tooth with a changed color. The carious cavity usually has a communication with the tooth canal. Significant pain is not probing, percussion can be slightly painful. When pressure is applied to the gum with the probe, it pales, a depression appears that persists for some time after pressing( vasoparesis).
- Radiography .X-ray examination is indispensable in differential diagnosis. The X-ray pattern fixes the darkened zone of rarefaction of the flame-shaped form in the tip of the root. The outlines of the dimming are not clear. There is an increase in the periodontal gap, the destruction of dentin and cement is visible.
- Electroodontometry .The method is based on the tactile and pain response of the pulpal receptors in response to the electrical current flowing through it. With granulating periodontitis, the excitability of the affected pulp reaches 100 μA and above.
Photo-x-ray photographing of patients with diagnosed granulomatous periodontitis:
Methods of treatment
Treatment of granulating periodontitis is carried out by surgical or endodontic( therapeutic) way.
Chronic stage
Treatment activities include the following steps:
- withdrawal from the focus of exudate inflammation;
- removal of an inflamed infected part - cleaning of the canal from decomposed pulp and infected dentin;
- destruction of pathogenic flora with antiseptics, resorbable antimicrobial and anti-inflammatory pastes embedded in the root of the tooth, if necessary, apply sulfonamides, broad-spectrum antibiotics, physiotherapy( ultrasound);
- measures are carried out to ensure the regeneration and recovery of affected bone structures and periapical tissues;
- filling of channels.
Surgical intervention if necessary.
Remission period
Physiotherapy and local anti-inflammatory drugs of complex action are used. Prescribed vitamins( mainly C and group B), biogenic stimulants.
Stage of exacerbation
Anesthesia is performed and treatment is carried out as in chronic course.
Surgical treatment
Teeth removed:
- with strong fracture of the crown part;
- with high mobility( III-IV stage);
- when it is impossible to open the channel due to its curvature, narrowing or obturation of the lumen.
Preference is given to operations that allow you to keep the tooth. These include: 
- amputation - removal of the affected root before the transition to the crown;
- hemisection - pruning the root of a multi-rooted tooth together with a crown;
- cystotomy - partial cyst removal;
- cystectomy - complete cyst removal;
- resection of the apex of the root - removal of the zone of infection and inflammation.
Prognosis and prevention of
 In 85% of cases, the correct treatment of granular periodontitis leads to complete tissue repair and tooth preservation as a functional unit. In the absence of treatment, the disease occurs with regular exacerbations, resulting in complete tooth removal.
In 85% of cases, the correct treatment of granular periodontitis leads to complete tissue repair and tooth preservation as a functional unit. In the absence of treatment, the disease occurs with regular exacerbations, resulting in complete tooth removal.
Prevention includes the elimination of risk factors, which include:
- lack of proper oral care;
- non-treatment of caries and pulpitis;
- scum deposits;
- smoking( cigarette smoke leads to the formation of biofilms, in which microorganisms are actively multiplying).
It is recommended that the diet be followed with an increase in plant rations in the diet, which ensures equal participation of all teeth in chewing. Regular visits to the dentist help prevent the transition of pulpitis and caries to periodontitis.