 Before talking about periodontitis, it is necessary to say a few words about periodontium, the most important part of the dentoalveolar system, which performs several important functions at once.
Before talking about periodontitis, it is necessary to say a few words about periodontium, the most important part of the dentoalveolar system, which performs several important functions at once.
Periodontitis is a thin connective tissue layer located between the root of the tooth and the alveolus. Its thickness is only 0.20-0.25 mm.
The functions of these tissues include:
- tooth retention in the alveolus( the main load is perceived by collagen fibers, one side embedded in dental cement, the other side is in the plate of the alveoli);
- uniform load distribution;
- protection of surrounding tissues and itself from foreign bodies;
- ensuring the correct metabolism.
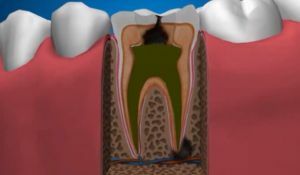
Periodontitis is an inflammation of the periodontal disease. It can be different in the clinic and the consequences, relatively harmless or threatening the very existence of the tooth. There are two main forms of periodontitis - acute and chronic. Depending on the nature of the flow periodontitis is granulating( granular), fibrous and granulomatous.
Any chronic periodontitis is accompanied by the formation of granulation tissue in place of the destroyed structures of the tooth and alveoli. However, the types of these formations, the clinic, and the consequences vary considerably.

The photo shows schematically the granulating( left) and granulomatous periodontitis( right)
In the granulomatous form of the disease, the focus of inflammation is placed in a fibrous capsule with a dense wall called granuloma.
This is one of its main differences from granulating periodontitis, in which the zone of destruction is not clearly encapsulated and is capable of rapidly increasing.
The risk of granulomatous periodontitis is between fibrous and granulating. The first is the most stable and safe, the second is the most dynamic and destructive.
Contents
- The causes and characteristics of the development
- The variety of forms
- The variety of forms
- The clinical features of
- Symptoms of the chronic and acute stage of the process
- Diagnosis and differentiation from similar processes
- Dental care
- Acute exacerbation
- Surgical treatment
- Consequences and preventive measures
- The clinical features of
Causes and features of development
GranulomatousPeriodontitis is a consequence of a granular process or develops independently. As already noted, the main feature of the granulomatous process is that the inflammation zone is enclosed in a fibrous capsule with a dense wall. This prevents the spread of infection from the diseased tooth to other organs and tissues. There is a kind of balance between pathogenic microflora, concentrated in the granuloma, and immunity.
At the site of the granuloma, the bone tissue of the tooth or alveoli is usually more or less destroyed. This is clearly visible on the x-ray. The focus of destruction has a well-defined oval or round shape. Around it formed compacted rim - the result of osteosclerosis.
Chronic granulomatous periodontitis sooner or later leads to the destruction of cement of the root and dental crown, and a gradual replacement by deposition in the form of a mace crowning the tip of the tooth. In appearance, the granuloma is similar to a bag of oval or round shape with a dense smooth shell, which is firmly attached to the roots.
Variety of forms of
Forms of periodontal inflammation differ in the phase in which they are( remission or exacerbation), as well as the shape and size of the lesion( granuloma, cystogranuloma or cyst).The difference is as follows: 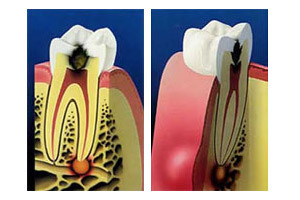
- Granuloma appears at the onset of the inflammatory process, and is a small( up to 0.5 mm) capsule-shaped foci of infection isolated from surrounding tissues by a dense membrane.
- The cystogranuloma is a 5-10 mm formation. Its important feature is the presence of epithelial cells lining the internal surface of the granuloma. Inside it creates an increased acidity, destroying the existing bone tissue and preventing the regeneration of a new one.
- The cyst is a fully formed, fluid-filled, cavity formation larger than 1 cm with the mucosa. Inside it there are cholesterol crystals. Their detection in exudate( with a cyst rupture or withdrawal through the fistula) with diffodiagnosis speaks in favor of the granulomatous process.
Features of the clinical picture
When remission, granulomatous inflammation occurs in a latent form and does not disturb the patient who does not see the reason for going to the doctor. In the absence of complications that occur relatively rarely, granulomatous periodontitis is often

. It can be seen in the photo that the granuloma appears on the x-ray as an
bead accidentally when an X-ray is examined for another disease. Fistulas, as a rule, are not formed.
With exacerbations, granulomatous periodontitis resembles sharp or sharpened granulating. There is a strong pain, there is a swelling of the adjacent tissues, lymphadenitis is noted, intoxication of the organism is increased.
When pressing on a sick tooth in the cyst, an increased pressure is created, which can lead to a disruption in the integrity of the capsule, the release of pus into the underlying tissues and the spread of infection.
Symptoms of the chronic and acute stage of the
process In the chronic course of the disease in the remission phase between the body's defenses and the infection localized in the cyst, there is a relative equilibrium that is disturbed by exacerbation.
The latter can occur with the activation of a destructive process due to a decrease in immunity. It is possible to melt the bone structures under the action of the contents of the cyst, a capsule can break and pus infection of neighboring tissues.
In case of complication, the size of the basal cyst and the zone of destruction can be so great that there is a risk of fracture of the jaw, even with minor trauma.
Diagnosis and differentiation from similar processes
Diagnosis is based on the clinic and hardware diagnostics data.
When a patient is questioned and a primary examination is made, the presence of pain, its nature and appearance time. Symptom, speaking in favor of granulomatous periodontitis, is the intensification of pain when nibbling. Examination of a diseased tooth allows to establish a change in its color, the presence of a carious cavity, hyperemia.

Probe is painless. ..
If there is a cyst on the surface of the jaw, a slight bulging may be palpable. Probing with granulomatous periodontitis is painless, the reaction to heat and cold can be either positive or negative. Questioning a patient about the time of discomfort or pain can make it possible to establish an acute or chronic character has a destructive process.
The basic hardware method for diagnosing periodontitis is radiography. She is able to answer almost all questions. In the granulomatous form of the disease, the radiograph shows a shaded area with a rounded configuration with distinct outlines in the apex zone.
Radiography is the most informative method for differential diagnosis. The focus of destruction in granular periodontitis does not have a clearly defined contour, but with fibrotic fixation only the periodontium extension is fixed.
Osteomyelitis is characterized by large areas of destruction, which are located outside the apex zone. Pulpitis and caries on the X-ray do not show any changes in the periodontium.
Diagnosis is really a very important stage of the entire treatment package:
Dental care
Treatment of granulomatous periodontitis depends on the type and size of the granuloma, the state of the dental canals( passable or not), as well as the state of immunity of the patient. If the destruction of bone structures is uncritical, and the body well resists inflammation, conservative treatment is performed.
- removes the destroyed structures of the tooth - necrotic pulp, infected dentin from the canal walls;
- destroys the pathogenic flora with the help of antiseptic agents introduced into the canal;
- activates the regeneration of damaged bone structures by the introduction of appropriate medications into the tooth;
- tooth is sealed.
An effective preparation with a bactericidal and regenerative action is Metapex, having a pH of 12.5.For a day, it destroys 90% of the pathogenic microflora and stimulates the formation of osteoblasts, from which subsequently formed osteocytes( normal bone tissue).

Actions for exacerbation of
The first action when exacerbating is blocking pain. Then exudate from the cyst or granuloma is withdrawn and antibiotics are prescribed. Further therapy is determined by the form of granulation formation - granuloma, cystogranuloma or cyst.
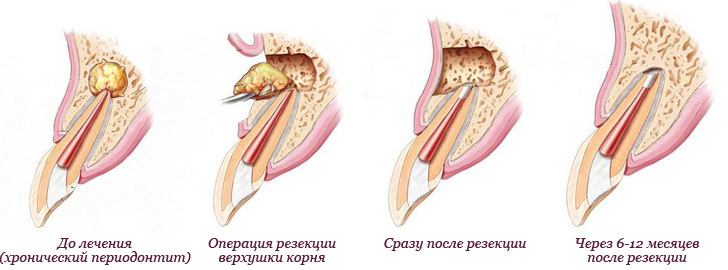
Surgical treatment
If surgical therapy is impossible, surgical treatment is performed, consisting in partial or complete removal of the tooth. Usually, as a tooth-preserving operation, resection of the apex of the root is performed. Access to it is made from the side of the gum( in the plate of the alveoli the window is cut).The affected apex of the root is cut, the formed space is filled with material regenerating bone tissue.
If the size of the granuloma is such that more than 1/3 of the root is required, the resection is discarded and the tooth is completely removed.
Consequences and preventive measures
The consequences of granulomatous periodontitis primarily depend on the timeliness of treatment and the correct treatment.
With competent conservative treatment of the disease in the stage of granuloma or cystogranuloma inflammation passes into the fibrous form and ceases to disturb the patient. The tooth is retained as a functional unit.
 If the call to the doctor occurred after a delay, and the granuloma developed into a cyst, the tooth should be removed. In the worst case, the cyst extends to the roots of adjacent teeth, which, depending on the extent of the lesion, will require appropriate treatment.
If the call to the doctor occurred after a delay, and the granuloma developed into a cyst, the tooth should be removed. In the worst case, the cyst extends to the roots of adjacent teeth, which, depending on the extent of the lesion, will require appropriate treatment.
The best prevention is to visit the dentist every six months. This is recommended to do, even if the teeth do not bother. The dentist will detect the disease at the earliest stages, if necessary, send for radiography.
The measures that prevent the development of periodontitis include:
- regular and daily oral care;
- timely treatment of caries and pulpitis;
- tartar control;
- quitting;
- adhering to a healthy diet.
Regarding the latter, the best food for maintaining teeth in a healthy state are tough vegetables and fruits, which provide a significant and even load on the dental apparatus.
