
System of tooth-periodontium, or in the embrace of careful but powerful
To understand what acute periodontitis is and why it develops, it should be realized that the tooth is not beaten into the gum and the jaw is tight, not hammered, like a nail in the board, but has enoughfreedom of movement in these structures due to the presence of ligaments between the jawbone and the tooth surface.
Bundles have the necessary power to hold the tooth in place, not allowing it to swing excessively back-to-back, left-to-right or rotate around the vertical axis. At the same time, by providing the tooth with the possibility of "springy squats" - limited by the elasticity of the ligaments in the hole up and down, they do not allow it to be pressed inwardly while chewing, keeping the jawbone from damage by this fairly solid formation.
In addition to the cushioning and fixing role, periodontal structures also perform the following functions: 
- protective, because they represent a histohematological barrier;
- trophic - providing communication with the body of the vascular and nervous systems;
- plastic - contribute to tissue repair;
- sensory - the implementation of all kinds of sensitivity.
With acute periodontal damage - periodontitis, all these functions are upset, which leads the patient to the door to the dentist's office at any time of the day. The symptoms are so acute that there is no thought even to "endure" and "wait out"( in contrast to the chronic course of the disease, when the sensations are quite tolerable).
content
- O mechanics destructive process, its steps
- Clinical symptoms basic forms
- Serous phase
- Purulent phase
- Traumatic form
- Drug form
- On the diagnosis and differentiation of other diseases
- Properties treatment
- First visit
- second visit in
- clinic in case of complications
- Possible consequences
- Preventative measures
About the mechanics of the destructive process, its stages
For the onset of acute neonatal periodontitiswalk or medicinal effect on periodontal tissue as in the treatment of pulpitis or pulpitis itself - penetration of infection into the tooth subsoil - the pulp. For this to occur, an entry is required to access the infection in the tooth cavity, the role of which is performed: the
- with an apical channel;
- cavity, protruded caries, or formed in the course of an insufficiently qualitatively sealed canal;
- by a line of damage resulting from an injury resulting in ligament rupture.
It is possible to get the infection through pathologically deep periodontal pockets.
From the damaged pulp, microbial toxins( or a preparation under the "arsenic" genesis of the condition) through the dentinal tubules leak into the periodontal gap, causing first the irritation of its structures, and then their inflammation.
The inflammatory process manifests itself: 
- pain due to the reaction of nerve endings;
- disorder of microcirculation, manifested by stagnant phenomena in tissues that outwardly look like their hyperemia and swelling;
- general reaction of the body to intoxication and other changes in its biochemistry.
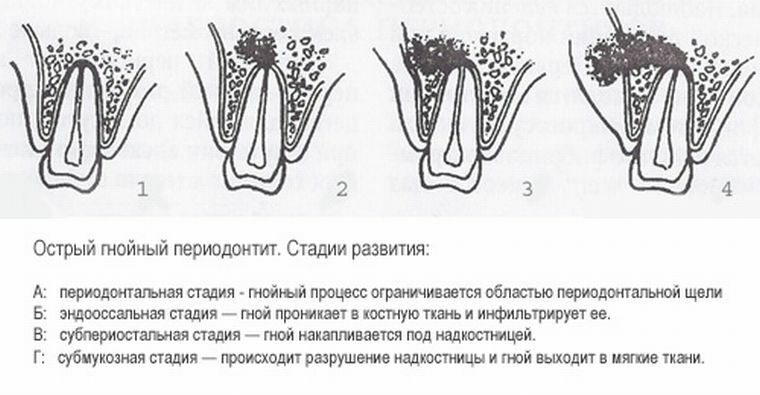
The destructive process passes through a series of successive successive stages:
- On , the periodontal stage of causes a focus( or several) that is separated from the intact zones of the periodontium. The focus is expanded, or merge into one smaller, with the involvement of a large volume of periodontal tissues. In view of the increase in tension in the closed volume, the exudate, looking for an outlet, breaks through either the marginal periodontal zone into the oral cavity, or by melting the compact plate of the dental alveolus into the bowels of the jaw. At this point, due to a sharp decrease in pressure exerted by the exudate, the pain is greatly weakened. The process goes into the next phase - it spreads under the periosteum.
- Subperiosteal( subperiosteal) phase, which exhibits symptoms of periostitis-flux with swelling in the oral cavity of the periosteum, which suppresses the pressure of the purulent exudate accumulated under it due to the density of its structure. Then, melting the periosteum, the pus appears under the mucous membrane, which is not a serious obstacle to its breakthrough into the oral cavity.
- In the third stage, in view of , the emergence of fistula - an apical joint with the oral cavity, the pain can almost completely disappear, or become insignificant, painful swelling in the apex projection disappears. The danger of this phase is that the inflammation does not end there, but continues to spread, capturing new zones, which can lead to serious consequences, including the development of osteomyelitis. Sometimes fistula formation means the transition of an acute condition to a chronic one.
Clinical symptomatology of the main forms of
Acute periodontitis in the composition of exudate is serous and purulent, and by the mechanism of occurrence:
- is infectious;
- is traumatic;
- is a medicament.
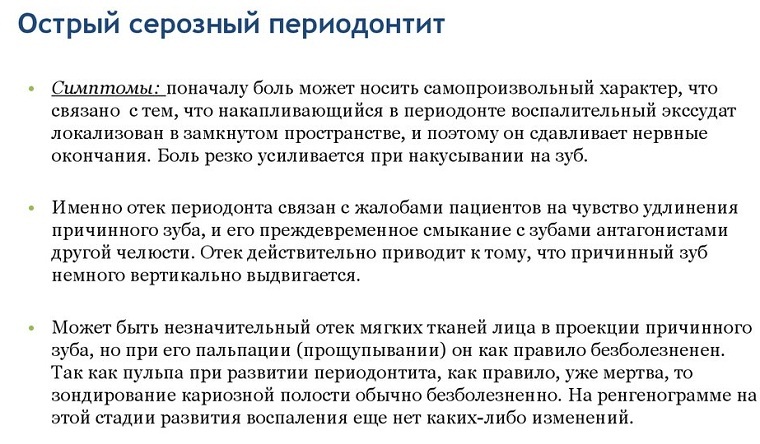
Serous phase
Serous periodontitis corresponds to the initial stage of the process - the sharpest nervous reaction of periodontal structures to their irritation with the appearance of initially small, but later more and more increasing changes.
Because of the increase in the permeability of the capillary walls, a serous effusion is formed, into which live and dead leukocytes, the products of vital activity of microbes, the remains of dead cells are then included. All this complex of microorganisms, active chemically and enzymatically, acts on the sensory nerve endings, causing their irritation, perceived as pain.
It has a permanent character, at first being blurred, but gradually and methodically increasing, becoming unbearable when it is beaten on the tooth. In some cases, prolonged and strong-willed pressing of the tooth by closing the jaws can lead to a reduction in pain manifestations( but without complete passage).There are no external manifestations in the environment of the affected tooth, because the inflammation in this case does not reach its peak.
Purulent phase of
If it is possible to overcome the initial pain without resorting to dental care, the process passes into the next phase of purulent melting, therefore periodontitis becomes purulent.
Foci of microabscesses form a single abscess, accumulated pus creates excess voltage in a closed volume, causing unforgettable and intolerable sensations to life.
 Characteristic symptoms are acute pain of a vomiting character, which irradiates into the proximal teeth and further, up to the opposite jaw. Even a slight touch to the tooth causes an explosion of soreness, a quiet closing of the mouth gives the effect of the greatest pressure on the affected area, a positive symptom of the "grown tooth" is in the absence of the reality of its protruding from the socket. The degree of fixation in the well decreases, temporarily and reversibly increasing the mobility of the teeth.
Characteristic symptoms are acute pain of a vomiting character, which irradiates into the proximal teeth and further, up to the opposite jaw. Even a slight touch to the tooth causes an explosion of soreness, a quiet closing of the mouth gives the effect of the greatest pressure on the affected area, a positive symptom of the "grown tooth" is in the absence of the reality of its protruding from the socket. The degree of fixation in the well decreases, temporarily and reversibly increasing the mobility of the teeth.
In the variant, when the entrance to the infection in the periodontal tissues is inadequately deep gingival pockets, they speak of the marginal form of periodontitis( as well as acute damage to the marginal periodontal disease).The gums become inflamed, bleeds occasionally, the process is accompanied by a copious discharge of pus right up to the suppuration with the corresponding odor of decomposition inherent in it.
In view of the active drainage, the pain in the general symptoms goes to the background, rather than with the apical form of pathology.
Acute purulent periodontitis under X-ray:
Traumatic form
In the case of a short-term action of great destructive force( as with an impact capable of causing rupture of ligaments over a large area), the development of traumatic periodontitis is possible. The intensity of pain depends on the degree of destruction of periodontal structures, significantly increasing when touched by the painful area.
The increased mobility is characteristic. With chronic negative effects periodontal tissues can be reconstructed, the resorption of the alveolar bone walls begins, the fixing ligaments collapse, which leads to the widening of the periodontal gap and loosening of the tooth.
Medication form
A distinctive feature of the medical form of the disease is its occurrence due to the effect on the periodontal structures of drugs introduced into the root canals mistakenly, or due to disorders with the use of therapeutic therapy.
The most commonly diagnosed is the development of arsenical periodontitis, which develops when the required dose of arsenic is exceeded for devitalization, and when it is too long to stay in the cavity of the tooth. The most popular "scenario" for the development of this form of the disease is the insufficient tightness of the temporary filling in the cervical cavity - the toxic drug should be immediately removed and the tissues treated with antidote( Unithiol).
Diagnosis and differentiation from other diseases
To diagnose, it is usually sufficient to question the patient( especially from a diagnostic point of view, signs of pulpitis in the past and significant tooth pain, sharply increasing from touch, in the present), plus objective research data( painlessness of sensing andspecific pattern of fracture of the crown).
Differentiate acute periodontitis with:
- with acute pulpitis;
- with chronic periodontitis in an exacerbation state;
- with osteomyelitis.

The pulpitis serves as a pulsating pain of paroxysmal property, its character and intensity do not change with percussion, but with a tendency to increase at night, periodontitis manifests itself as pain that does not pass through and is intolerable, tearing and sharply increasing from touching tissues.
In contrast to chronic periodontitis, the X-ray diffraction data for the acute process in periodontitis do not show.
When osteomyelitis in the image there is a vast extent of damage with the capture of the roots of neighboring teeth. Confirms the reliability of the diagnosis of the soreness of several neighboring teeth during percussion.
Features of treatment
The strategy of treatment of the acute phase of periodontitis involves two options: complete recovery of all cavities of the tooth with cleaning them from infection and decay products or, as an extreme measure, its removal along with all pathological contents.
After confirmation of the diagnosis, endodontic treatment of acute periodontitis is carried out, for which the best possible anesthesia is performed because of the extreme susceptibility of inflamed tissues to touch and vibration.
First visit to
The first visit to the clinic removes the defect of the tooth crown by dissecting it to healthy tissues, in the presence of already installed seals, they are removed. 
The next step is the discovery and opening of the mouths of the root canals. In the case of their previous sealing, the material of the fillings is removed, and when the channels are first opened, the detritus is removed as thoroughly as possible, the walls are machined mechanically with the excision of all non-viable tissues. In parallel, the lumen of the canals is expanded to a diameter sufficient for further passage and sealing.
All procedures are performed using an antiseptic solution( Sodium hypochlorite or Chlorhexidine bigluconate).
After the creation of a sufficiently reliable drainage, the treatment of the apical region involves the fulfillment of three tasks:
- , the destruction of the diseased flora in the main cavities of the roots;
- extermination of infection in all branches of the root canals up to the dentinal tubules;
- suppression of the periodontal focus of inflammation.
The success of these events is facilitated by the use of:
- electrophoresis with one of the antiseptic solutions;
- method of intensifying diffusion into the root canals of therapeutic agents using ultrasound techniques;
- treatment of root canals by laser irradiation( the effect is achieved by combining radiation with the bactericidal action of atomic oxygen or chlorine released from specially applied solutions under the influence of a laser).
Completes the stage of machining and antiseptic dressing of the tooth canals leaving it unclosed for 2-3 days. The doctor gives recommendations to the patient on the scheme for taking antibacterial drugs and the use of rinsing with medicinal solutions.
With signs of periostitis, the cavity is opened with an indiscriminate cutting of the periosteum along the transitional fold in the area of the root apex projection, with obligatory jet washing with an antiseptic solution and closure of the wound with elastic drainage.
Second visit to the clinic
On the second visit to the dental clinic in the absence of the patient's complaints, the canal is filled either permanently or temporarily for a period of 5-7 days using Calcium hydroxide to treat the outside space. In this case, the installation of a permanent root filling and the reconstruction of the crown are postponed until the third visit.
In the case of complications of
If the root canal is obstructed or if endodontic treatment fails, the tooth is removed with further recommendations to the patient on the tactics of treating the alveoli at home.
When examined on the next day( if necessary), the wells are cleaned of the remaining convolutions of blood with a loose tamponade with a bandage covered with iodoform, with repetition of the manipulation after 1-2 days. In the absence of symptoms of the alveolitis, there is no need for additional manipulation.
The occurrence of "arsenic periodontitis" requires the immediate removal of a toxic agent with the treatment of inflamed tissues with an antidote.
Possible consequences of
If the treatment of acute periodontitis was carried out professionally, the prognosis does not cause concern.
If there is no timely request for dental care or if the measures taken are unsuccessful, the possible consequences are as follows:
- development of periostitis, phlegmon or abscess in the tissues of the gums and jaw( up to osteomyelitis);
- transition process from acute to chronic with the formation of a cyst or granuloma.
Preventive measures
Preventative measures include careful treatment of teeth in compliance with all hygiene standards, regular visits to the dentist.
 The prevention of the development of caries and its unchanging companion pulpitis is possible only when following the norms of common sense in the process of chewing, because only a healthy periodontium successfully resists the loads developed by all groups of masticatory muscles.
The prevention of the development of caries and its unchanging companion pulpitis is possible only when following the norms of common sense in the process of chewing, because only a healthy periodontium successfully resists the loads developed by all groups of masticatory muscles.
To avoid the development of medical periodontitis, strict adherence to norms and procedures is necessary in the treatment of oral diseases, prosthetics, as well as restoring normal bite, should be performed without undue burden on periodontium.
Any endodontic operation must be completed with a full obturation of root canals along their entire length. In the case of not fully traversed channels or poor-quality filling, the development of pulpitis, followed by periodontitis, is inexorable.
