
Schintz disease or Haglund-Schintz deformity was studied by a Swedish surgeon back in 1927.It is also known as osteochondrosis of the apophyses of the calcaneus, osteochondropathy, deformation of Mulholland. From what there is a disease of Shinz till now till the end and it is not revealed. Usually, this disease manifests itself after long physical activity or as a result of previous trauma.
- What disease Shintsa
- reasons
- Symptoms
- Stage
- Diagnostics
- Treatment
- Conservative
- Physiotherapy
- Therapeutic exercise
- Exercises
- Massage
- Folk remedies
- packs
- Applications
- Surgery
- removal growths
- wedge osteotomy
- Consequences
- Prevention
What is Schintz disease
This disease, in most cases, occurs in those who are actively involved in sports, includingand professional. Diseases are both adults and children.
Haglund-Schintz deformation is a bone growth on the back of the heel, when the process of ossification is disturbed in the heel of the calcaneus. Shinz's disease usually develops in those who in everyday life prefer tight and tight shoes with closed heels. The risk of developing Haglund's deformity also depends on the shape of the calcaneus.

This disease is an anomaly of bones and soft tissues of the foot. This causes the increase in the bone part of the heel, in the part where the Achilles tendon is located. Soft tissues near the back of the heel can get annoyed when a large bony piece rubs against tight and tight shoes. This often leads to bursitis, that is, inflammation of the fluid-filled sac between the tendon and the bone. When the heel is inflamed, calcium can accumulate in it, which increases pain. To facilitate this condition, both surgical and non-surgical therapies are available.
to table of contents ^Reasons for
Schintz disease can develop for the following reasons:
- Active sports activity, including professional ( football, running and the like) and a constant load on the muscles of the legs.
- Wearing stiff shoes with closed heels .
- Incorrect selection of high-heel shoes .Women aged 15-35 who prefer to wear high-heel shoes above 5 cm have a high Haglund strain deformation rate. It is believed that the pressure on the Achilles tendon and the retrocalcaneal bursa is aggravated by the height of the heel.
- Constant pressure It can cause painful irritation in the bursa and other tissues at the back of the foot such as the Achilles tendon.
- Hereditary factors of leg development can contribute to its development, although Schintz's disease is not a hereditary disease.
- High arches of the .Achilles tendon or heel tendon is the most powerful tendon in the body, it connects the leg muscles to the calcaneus. A high arch of the arch of the foot occurs when the heel bone emerges from the position and tilts back to the Achilles tendon. The result of the high arch is that the heel bone actually rubs against the tendon, causing irritation. Over time, the heel bone begins to deform and rub against the seminary. Bursa is a fluid-filled sac, the purpose of which is to eliminate friction between the tendon and the calcaneus. When the bursa is irritated, it becomes inflamed and can cause considerable pain.
- Thick Achilles tendon .The bursa lies between the Achilles tendon and the calcaneus. If the Achilles tendon is very rigid and inflexible, it can put pressure on the bursa. Constant pressure can also lead to inflammation and pain from the bursa.
- Pronation of the foot .Walking on the outside of the foot causes internal rotation of the heel. In this case, the bursa can form under the tendon, in order to reduce the friction caused by abnormal turn of the leg. Bursa is under such pressure that it inflames and causes pain.
What contributes to the development of the disease:
- microtrauma, which are formed in the heel area, the cause of this is poor blood supply;
- vascular disease;
- is a neuro-trophic disorder;
- disrupted body assimilation by Ca;
- endocrine system diseases associated with hormonal imbalance;
- frequent load on the legs;
- genetic predisposition.
These factors of the development of the disease are typical for both adults and children.
Symptoms of
The manifestation of Haglund deformation is possible in one or both stops. Symptoms may be of the following nature:
- formation of bone growth on the back of the heel;
- severe pain in the heel;
- swelling in the bursa;
- pain after a while beginning any activity that subsides with increasing activity;
- pain or swelling in the heel;
- redness of the heel;
- attenuation or total absence of pain during sleep, or when the leg is at rest;
- it is difficult to bend and unbend the foot;
- the person starts to noticeably limp.
The disease can manifest itself with time, and develop rapidly. In the acute stage, the disease is characterized by a sharp pain, which gradually increases in the area of the calcaneus, especially it is felt after the load. For example, if a person ran for a long time or had to walk a lot.
A little above the calcaneal knoll, there is swelling, there is a aching pain, while bending the foot or stretching it is uncomfortable. The patient moves sluggishly, while walking like "on socks."
Stages of
There are several stages of Shinz's disease:
- Aseptic necrosis of .The feeding of the bone site is disturbed, which leads to a foci of necrosis.
- Impression fracture of the .The affected area does not withstand the usual load, the pressure of one part of the bone occurs on the other.
- Fragmentation of .There is a division of the affected area into separate fragments.
- Necrotic tissue dissolves .
- Reparation of .The site of necrosis subsequently ossifies.
Diagnosis
It is performed only by a specialist - an orthopedic physician. It takes into account the clinical picture, anamnesis and the result of one or more studies of the foot images.
Radiography, ultrasound or magnetic resonance imaging( MRI) are used by the orthopedist to exclude other causes of leg pain. It is best if a picture taken in the lateral projection is assigned.
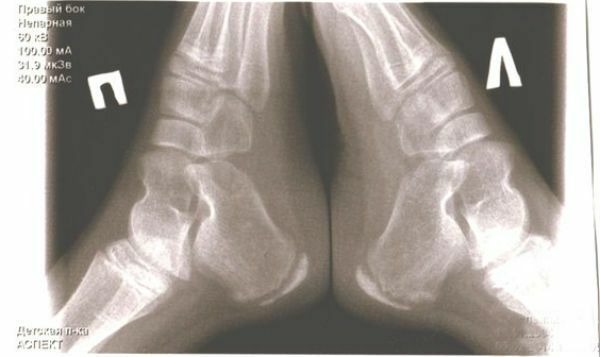
X-ray signs include:
- apophysing seal;
- the gap between the apophysis and calcaneus is enlarged;
- The compacted ossification spot has a patchy structure.
Treatment of
Treatment of Haglund deformity can be divided into two types: non-surgical and surgical. In a larger percentage, treatment usually begins with more sparing measures. Surgery is used only when all other measures can not solve the problem, pain increases, making walking more difficult.
to contents ^Conservative
The patient is first restricted to physical activity. If the pain is markedly increased, then the diseased limb is fixed with a tape made of gypsum, for short periods of time. In severe pain syndrome, the doctor prescribes the use of analgesics and physiotherapy, for example, ointments. Helps with the treatment and adoption of warm baths.
In order to reduce the burden on the heel and the entire foot as a whole, doctors recommend wearing orthopedic insoles and heel pads with gel.
Non-surgical options include:
- Wearing shoes solely without a heel, such as clogs, or sandals.
- Admission of non-steroidal anti-inflammatory drugs( NSAIDs) such as Ibuprofen or Aspirin.
- Wearing orthopedics.
- Wearing gel or silicone hips, insoles, to reduce the pressure of normal shoes.
- Wearing immobilizing dressings or cast shoes.
- Cold compression therapy;
- In case of pain, vitamins of group B are also prescribed.
Physiotherapy
To eliminate the disease the doctor can prescribe the passage of such physiotherapy procedures as:
- diathermy;
- electrophoresis with pyrogen, lidocaine or lidase;
- therapy using magnets;
- ultrasound with hydrocortisone;
- shock wave therapy.
ozocerite and paraffin applications;
Physiotherapy
This therapy can only be used after the acute pain has already passed. It must be remembered that for each patient the complex of exercises is selected individually and exclusively by the doctor. Physiotherapy helps to reduce pain, strengthens and stretches muscles, and significantly improves the flow of blood in the veins.
For example, exercises for Achilles tendon - this is the best form of exercise for the treatment of Schintz disease. They can be performed in cases where the Achilles tendon is too tight. Stretching the calf muscle can weaken it. If you exercise regularly, you can prevent the development of Haglund's syndrome.
to contents ^Exercises
- Sit down and put a sore foot on the knee of the second limb. Rotate the foot of the affected leg at a moderate pace for a few seconds. The tempo can be increased by counting up to 16-30 rotations.
- Stand on a hard, smooth surface and lift your toes up. Do this slowly, then move your fingers so that from the heels to the arch rising the foot remains on the floor. Hold in this position for 10 seconds, then relax and repeat the exercise several times.
- Sit on a chair so that the knees are in a straight line and connect the feet. Then repeat the exercise again.
- Sit on a chair and lift it up alternately, and then lower your toes so that the heel is still.
- Lie on the floor sideways, so that the sick heel is closer to the floor. If the right foot is hit, then lie down on the right side, if the left one is on the left. Put your hand in the elbow, put it under your head. Pull out the leg that is on top to the side. Raise the foot of the affected limb slightly and rotate clockwise, without lifting it from the floor. Do this exercise takes about 1 minute.
Massage
To treat Shinz's disease, a therapeutic massage is applied, in which the heel zone is necessarily weeded. In terms of intensity, massage should be moderate. Massage should be done every day, throughout the crescent. After a break in a month and a half, the course is resumed.
Folk remedies
It is possible to resort to folk remedies only after acute pain syndrome has passed. It must be remembered that there are no folk methods of treating Shinz's disease, they can only reduce pain. Often at home, the following substances are used:
- Iodine .This is an excellent remedy, which you can smear the affected area or use it as compresses. It will help to remove pain, and also to remove inflammation.
- Soap and iodine mesh .Grate the soap on a grater and put on a lump, after a while wash off and draw an iodine lattice.
- Potatoes .Purification of potatoes must be welded and in this broth soar your feet. When the broth cools down, pour hot water. This is a very simple way that you can do daily.
- Propolis .It is known for its anti-inflammatory and antibacterial properties. A small ball needs to be stretched and applied to the heels, doing this every day.
- Baths with essential oils and medicinal herbs.
- Baths with sea salt.
Compresses
The warming compresses will help you to get rid of the pain. Usually apply a compress with dimexid, which is sold in a pharmacy. It is mixed with water in a ratio of 1: 1.The resulting solution is applied with a moistened gauze pad, which is applied for a period of 30 minutes to 1 hour. A polyethylene film is applied over the gauze napkin and wrapped with a warm woolen cloth. When the warming compress is removed, an anti-inflammatory ointment can be applied to the heel.
to contents ^Applications
Ozokerite and paraffin applications also help. Such procedures can be done both in the hospital and at home. This medicinal substance has a mountain origin. It is a waxy product, which includes organic resins, hydrocarbon, ozocerite rod and asphaltenes, which act like antibiotics.
The essence of such applications is that during their heating and application to the affected area, the thermal effect contributes to the enhancement of peripheral blood flow and a decrease in muscle tone.
For carrying out the appliance at home, the following steps are taken.
- Ozokerite and paraffin are placed in a saucepan in equal proportions, and put on a water bath( about 1 hour).
- The resulting mixture is poured into a flat shape that will create an application thickness of 1.5 centimeters. If the paraffin remains a depression by pressing, it is ready for use.
- To perform the application over the blanket, a diaper, and then an oilcloth, on which the paraffin wax is laid. It is put on the affected heel, which must be wrapped in the reverse order.
- Application should be kept for 15 to 30 minutes.
Surgical intervention
It is used to treat Haglund's deformity if less invasive methods do not work. During surgery, the doctor removes the extra bone from the heel. It can also be smoothed and ground. This reduces pressure on the bursa and soft tissues.
to table of contents ^Removing outgrowths of
Many surgeons simply remove the build-up. This procedure is performed through a small incision at the back of the heel. Achilles tendon moves away, so that the surgeon can see the back of the calcaneus. Then some part of the bone is removed, and the heel shape is formed and rounded, so that pressure does not occur. The incision is closed with stitches, and the leg is placed in a bulky bandage to protect it until healing. It can also be placed on the tire from the knee to the toes.
to table of contents ^Vaginal osteotomy
This procedure is the same as removing the outgrowths. General anesthesia may be given during surgery. This is usually done if the Achilles tendon is damaged, and the doctor needs to fix it.
After the operation, it will take up to 8 weeks for complete recovery. Most likely, you will have to wear a special shoe to protect your leg, and use crutches.
to contents ^Consequences of
It is extremely important for a person suffering from Schintz's disease to stop the activity that led to the development of this syndrome for at least 1 month. The rest period is assessed depending on the severity of the injury. For ranks I and II types of injuries caused by Schintz disease, the rest period and recovery is about a week, and for more serious injuries, the recovery period increases to about a month. During this period it is extremely important to stop any sports activity.
Remember that after reducing pain, the load can be restored, but while wearing shoes with a wide and stable heel only. But the shoes on flat shoes will have to be abandoned, since it increases the load on the heel.
Prevention of
Preventing Haglund deformation or preventing relapse after treatment means taking action to treat any other existing foot damage and avoiding irritation of the Achilles tendon and bursa. Low-heeled shoes with a flexible back that supports the arch of the foot can help prevent bursitis from recurrence.
To reduce the risk of developing Shinz's disease, you can, following the following recommendations:
- avoid wearing shoes with tight, stiff heels, especially for long periods of time;
- avoid running on hard surfaces or uphill;
- wear open shoes;
- wear soft socks with a non-slip sole;
- perform stretching exercises to prevent tightening of the Achilles tendon.
- Avoid repetitive movements in the foot and ankle, especially on a hard surface.
- avoid sports shoes that compress the retrocalcaneanal bursa and Achilles tendon during sports( from runners, from golf shoes or hockey skates).
- to avoid wearing high heels, since such shoes exert pressure on the retrocalcaneanal bursa and Achilles tendon, causing Schintz's disease.
As practice shows, the treatment of Shinz's disease in the early stages prevents its "transformation" into a chronic disease. With proper treatment, the pain should disappear. Usually it is about a term of 1.5-2 years. Pain may persist for a longer time, but with proper treatment and compliance with all recommendations, the outcome of Shinz's disease will be a complete recovery.
